
Torticollis (टॉर्टिकोलिस / गर्दन टेढ़ी)
Torticollis (Wryneck) Treatment
शिशु में गर्दन टेढ़ी होने का विशेषज्ञ उपचार - Physical Therapy, Stretching, Surgery | Indore
Expert Treatment for Infant Neck Tilting - Physical Therapy, Stretching, Surgery | Indore
Torticollis क्या है?
What is Torticollis?
Torticollis (टॉर्टिकोलिस) एक ऐसी स्थिति है जिसमें शिशु या बच्चे की गर्दन एक तरफ झुकी या टेढ़ी हो जाती है। इसे "Wryneck" (रिंक नेक) भी कहा जाता है। यह सबसे आम pediatric orthopedic समस्याओं में से एक है।
🎯 मुख्य लक्षण:
- गर्दन का एक तरफ झुकना: बच्चे का सिर लगातार एक तरफ झुका रहता है
- गर्दन घुमाने में कठिनाई: दूसरी तरफ देखने में परेशानी
- मांसपेशी में गांठ: गर्दन में एक तरफ सख्त गांठ महसूस होना
- चेहरे की असमानता: लंबे समय तक रहने पर चेहरा असमान हो सकता है
यह स्थिति ज्यादातर जन्म के समय या जन्म के तुरंत बाद दिखाई देती है। अच्छी खबर यह है कि 90% से अधिक मामले physical therapy और stretching exercises से ठीक हो जाते हैं!
Torticollis is a condition where an infant's or child's neck is twisted or tilted to one side. It's also called "Wryneck." This is one of the most common pediatric orthopedic problems.
🎯 Key Features:
- Head tilted to one side: The child's head persistently tilts to one side
- Difficulty turning neck: Trouble looking to the opposite side
- Neck muscle lump: A hard lump felt on one side of the neck
- Facial asymmetry: Face may become uneven if left untreated long-term
This condition mostly appears at birth or shortly after birth. The good news is that over 90% of cases resolve with physical therapy and stretching exercises!
Torticollis के प्रकार
Types of Torticollis
Congenital Muscular Torticollis (CMT)
सबसे आम प्रकार! जन्म के समय मौजूद होता है। SCM (Sternocleidomastoid) muscle में समस्या के कारण होता है। प्रसव के दौरान मांसपेशी में खिंचाव या रक्त प्रवाह में कमी से होता है। यह लगभग 85-90% cases में होता है।
Congenital Muscular Torticollis (CMT)
Most common type! Present at birth. Caused by problem in SCM (Sternocleidomastoid) muscle. Occurs due to muscle stretching or reduced blood flow during delivery. Accounts for approximately 85-90% of cases.
Acquired Torticollis (बाद में होने वाला)
जन्म के बाद develop होता है। कारण: गर्दन में चोट, संक्रमण, inflammation, lymph nodes की सूजन, या गर्दन की गलत positioning। इसे जल्द पहचान कर treatment जरूरी है।
Acquired Torticollis
Develops after birth. Causes: neck injury, infection, inflammation, swollen lymph nodes, or poor neck positioning. Early identification and treatment are essential.
Positional/Postural Torticollis
लंबे समय तक एक ही position में लेटने से होता है। मांसपेशी में कोई structural problem नहीं होती। सबसे आसानी से ठीक होने वाला प्रकार! Positioning changes और simple exercises से ठीक हो जाता है।
Positional/Postural Torticollis
Caused by lying in the same position for long periods. No structural muscle problem. Easiest type to correct! Resolves with positioning changes and simple exercises.
Spasmodic Torticollis (Adults में)
ज्यादातर adults में होता है। गर्दन की मांसपेशियों में अनियंत्रित spasms होते हैं। यह एक neurological disorder है जिसे cervical dystonia भी कहते हैं। Botox injections से treatment होता है।
Spasmodic Torticollis (In Adults)
Mostly occurs in adults. Uncontrolled spasms in neck muscles. It's a neurological disorder also called cervical dystonia. Treated with Botox injections.
🩺 सबसे महत्वपूर्ण बात:
Congenital Muscular Torticollis (CMT) शिशुओं में सबसे आम है और इसका treatment सबसे successful होता है। जितनी जल्दी treatment शुरू हो, उतना बेहतर परिणाम मिलता है!
🩺 Most Important Point:
Congenital Muscular Torticollis (CMT) is the most common in infants and has the most successful treatment outcomes. The earlier treatment begins, the better the results!
कारण क्या होते हैं?
What Causes Torticollis?
🧬 Congenital Torticollis के कारण:
- Difficult delivery: प्रसव के दौरान मांसपेशी में खिंचाव या चोट
- Breech position: गर्भ में बच्चे की गलत position
- Multiple births: जुड़वां या तीन बच्चे होने पर गर्भाशय में कम जगह
- Reduced blood flow: प्रसव के दौरान मांसपेशी में रक्त प्रवाह कम होना
- Fibromatosis colli: SCM muscle में fibrosis (scarring) होना
- In-utero crowding: गर्भ में बच्चे के सिर की positioning
🔄 Acquired Torticollis के कारण:
- Trauma: गर्दन में चोट लगना
- Infection: गले या गर्दन में infection (pharyngitis, cervical adenitis)
- Inflammation: मांसपेशियों या joints में सूजन
- Tumor: दुर्लभ मामलों में tumor (बहुत कम होता है)
- Vision problems: आंखों की मांसपेशियों में समस्या
- Poor positioning: लंबे समय तक गलत position में सोना
⚠️ ध्यान दें:
अगर torticollis अचानक बड़े बच्चे या adult में develop हो, तो यह किसी serious underlying condition का संकेत हो सकता है। तुरंत doctor से consult करें!
🧬 Causes of Congenital Torticollis:
- Difficult delivery: Muscle stretching or injury during birth
- Breech position: Abnormal fetal position in the womb
- Multiple births: Limited space in uterus with twins or triplets
- Reduced blood flow: Decreased blood flow to muscle during delivery
- Fibromatosis colli: Fibrosis (scarring) in SCM muscle
- In-utero crowding: Head positioning in the womb
🔄 Causes of Acquired Torticollis:
- Trauma: Neck injury
- Infection: Throat or neck infection (pharyngitis, cervical adenitis)
- Inflammation: Muscle or joint inflammation
- Tumor: In rare cases, tumor (very uncommon)
- Vision problems: Eye muscle problems
- Poor positioning: Sleeping in wrong position for extended periods
⚠️ Important:
If torticollis suddenly develops in an older child or adult, it may indicate a serious underlying condition. Consult a doctor immediately!
लक्षण और पहचान
Symptoms & Diagnosis
👀 प्रमुख लक्षण:
सिर का झुकाव
बच्चे का सिर लगातार एक तरफ झुका रहता है (ear towards shoulder)
घुमाने में कठिनाई
गर्दन को दूसरी तरफ घुमाने में परेशानी या बच्चा एक ही तरफ देखता है
गांठ महसूस होना
गर्दन में एक तरफ sternocleidomastoid muscle में सख्त गांठ
चेहरे की असमानता
Long-standing cases में चेहरे का एक side थोड़ा flat हो सकता है
Feeding में दिक्कत
एक तरफ से feeding करने में परेशानी
आंखों की movement
बच्चा गर्दन घुमाने की बजाय केवल आंखें घुमाता है
🔬 डायग्नोसिस कैसे होता है?
- Physical Examination: Doctor गर्दन की movement, muscle की tightness, और गांठ की जांच करते हैं
- Ultrasound: SCM muscle की internal structure देखने के लिए
- X-rays: Spine या bone की abnormality rule out करने के लिए
- Hip Ultrasound: 20% cases में hip dysplasia भी होता है, इसलिए hip screening जरूरी
- Eye Examination: Vision problems rule out करने के लिए
✅ शुरुआती पहचान:
ज्यादातर cases में torticollis जन्म के 2-4 हफ्तों के भीतर पहचाना जा सकता है। जितनी जल्दी पहचान हो, उतना बेहतर परिणाम मिलता है!
👀 Main Symptoms:
Head Tilt
Child's head persistently tilted to one side (ear towards shoulder)
Difficulty Turning
Trouble turning neck to the opposite side or child only looks one way
Lump Felt
Hard lump in sternocleidomastoid muscle on one side of neck
Facial Asymmetry
In long-standing cases, one side of face may appear slightly flat
Feeding Difficulty
Trouble feeding from one side
Eye Movement
Child moves only eyes instead of turning neck
🔬 How is it Diagnosed?
- Physical Examination: Doctor checks neck movement, muscle tightness, and lump
- Ultrasound: To view internal structure of SCM muscle
- X-rays: To rule out spine or bone abnormalities
- Hip Ultrasound: Hip dysplasia occurs in 20% of cases, so hip screening is essential
- Eye Examination: To rule out vision problems
✅ Early Detection:
In most cases, torticollis can be identified within 2-4 weeks of birth. The earlier it's detected, the better the outcome!
उपचार के विकल्प
Treatment Options
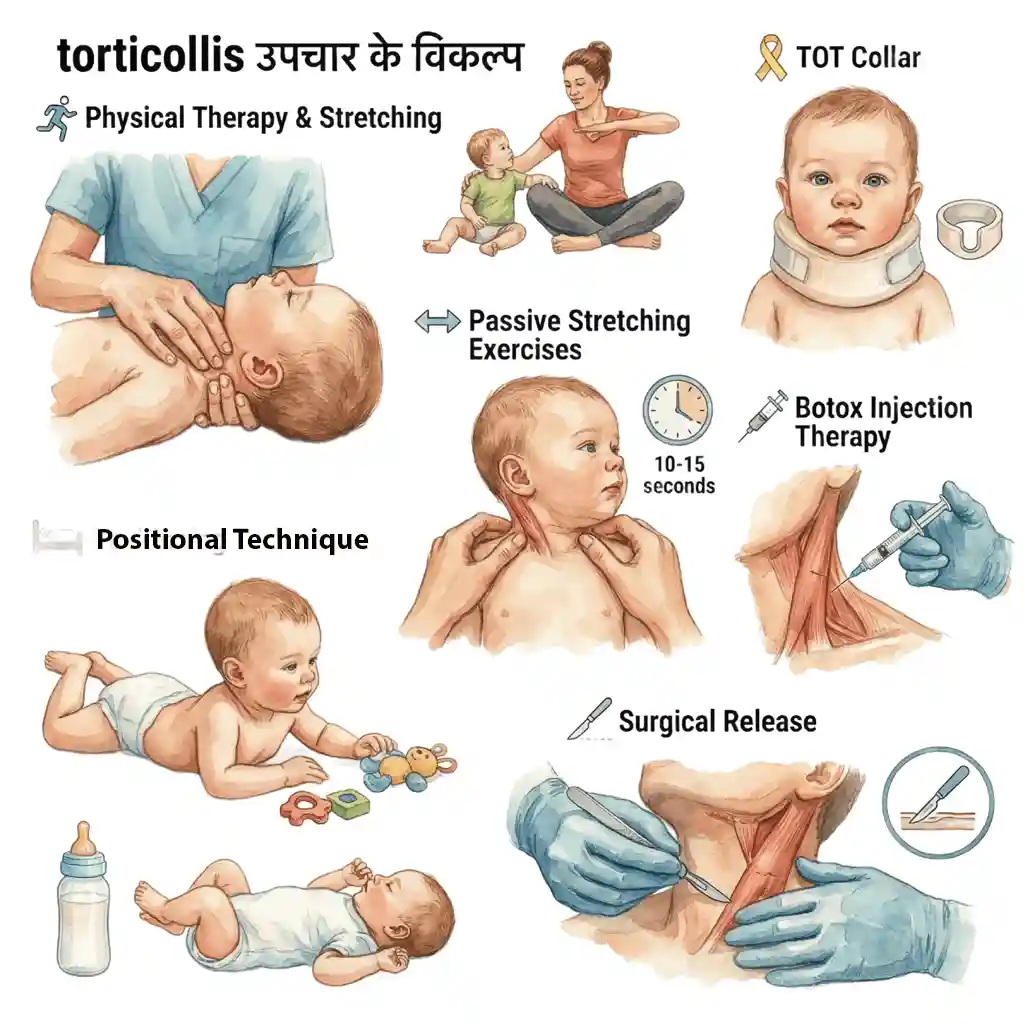
Physical Therapy & Stretching
सबसे महत्वपूर्ण treatment! Trained physiotherapist द्वारा gentle stretching exercises। Daily home exercises program। 90% cases में successful। 3-6 महीने में improvement। Parent education जरूरी। Consistency key to success!
Physical Therapy & Stretching
Most important treatment! Gentle stretching exercises by trained physiotherapist. Daily home exercise program. Successful in 90% of cases. Improvement in 3-6 months. Parent education essential. Consistency is key to success!
Positioning Techniques
बच्चे को सही position में रखना। Toys affected side पर रखें ताकि बच्चा गर्दन घुमाए। Feeding time पर opposite side use करें। Sleep positioning - alternate head position। Tummy time encourage करें। Active range of motion बढ़ाने में मदद!
Positioning Techniques
Proper positioning of baby. Place toys on affected side to encourage neck turning. Use opposite side during feeding time. Sleep positioning - alternate head position. Encourage tummy time. Helps increase active range of motion!
Passive Stretching Exercises
Parents द्वारा दिन में 4-5 बार gentle stretching। SCM muscle को carefully stretch करना। Each stretch 10-15 seconds hold। Never force! Gradual progress। PT sessions में सीखना जरूरी। Daily consistency से best results मिलते हैं।
Passive Stretching Exercises
Gentle stretching by parents 4-5 times daily. Carefully stretch SCM muscle. Hold each stretch 10-15 seconds. Never force! Gradual progress. Learning in PT sessions is essential. Daily consistency gives best results.
TOT Collar (Tubular Orthosis for Torticollis)
Special collar जो सिर को सही position में रखता है। Moderate से severe cases में use होता है। Daily कुछ hours पहनना। PT के साथ combination में effective। Not for all cases - doctor की सलाह जरूरी।
TOT Collar (Tubular Orthosis for Torticollis)
Special collar that keeps head in correct position. Used in moderate to severe cases. Worn for several hours daily. Effective in combination with PT. Not for all cases - doctor's advice necessary.
Botox Injection Therapy
Selected cases में जब PT response नहीं मिलता। SCM muscle में injection। Muscle को relax करता है। Stretching आसान बनाता है। Temporary effect - 3-6 months। PT के साथ combined therapy। Adult spasmodic torticollis में भी effective।
Botox Injection Therapy
For selected cases when PT doesn't respond. Injection into SCM muscle. Relaxes the muscle. Makes stretching easier. Temporary effect - 3-6 months. Combined therapy with PT. Also effective for adult spasmodic torticollis.
Surgical Release
Last resort! केवल 5-10% cases में जरूरी। जब conservative treatment fail हो। Age > 1 year और persistent tightness। SCM muscle release surgery। Craniofacial asymmetry correction। Post-surgery intensive PT जरूरी। Success rate बहुत high!
Surgical Release
Last resort! Necessary in only 5-10% of cases. When conservative treatment fails. Age > 1 year with persistent tightness. SCM muscle release surgery. Craniofacial asymmetry correction. Post-surgery intensive PT essential. Success rate very high!
✅ महत्वपूर्ण बातें:
- जल्दी शुरुआत करें: 3-6 महीने की age तक treatment start करना ideal
- Consistency जरूरी: Daily exercises और positioning बहुत important
- 90% Success Rate: Physical therapy से ज्यादातर cases ठीक हो जाते हैं
- Surgery rarely needed: केवल 5-10% cases में surgery की जरूरत
- Regular follow-up: Progress monitor करने के लिए doctor visits जरूरी
✅ Important Points:
- Start early: Starting treatment by 3-6 months of age is ideal
- Consistency matters: Daily exercises and positioning very important
- 90% Success Rate: Most cases resolve with physical therapy
- Surgery rarely needed: Only 5-10% of cases require surgery
- Regular follow-up: Doctor visits necessary to monitor progress
सर्जिकल मैनेजमेंट (Surgical Management)
Surgical Management
⚠️ महत्वपूर्ण:
Surgery केवल 5-10% cases में जरूरी होती है। यह LAST RESORT option है जब conservative treatment (PT, stretching) 6-12 महीने तक fail हो जाए। Dr. Gaurav Jain experienced pediatric orthopedic surgeon हैं जो torticollis surgery में expert हैं।
🎯 Surgery के Indications (कब जरूरी है?):
Age > 12-18 Months
बच्चे की age 12-18 महीने से ज्यादा हो और persistent tightness रहे। यह ideal surgical age window है क्योंकि इस समय तक conservative treatment का adequate trial हो चुका होता है।
Failed Conservative Treatment
कम से कम 6 months तक intensive PT और stretching के बावजूद कोई significant improvement नहीं। Range of motion में 30 degrees से कम improvement। SCM tightness persistent रहना।
Severe Contracture
SCM muscle में severe fibrosis और contracture। Passive stretching से भी adequate ROM नहीं मिल पाता। Muscle permanently shortened हो गई है और fibrous tissue बन गई है।
Craniofacial Asymmetry
चेहरे और सिर में significant asymmetry develop हो गई है। Plagiocephaly (flat head) progressive हो रहा है। Facial bones असमान develop हो रहे हैं। Cosmetic concern बढ़ रही है।
Secondary Problems
Vision problems develop होने लगें। Cervical spine में secondary deformity। Shoulder girdle asymmetry। Functional limitations daily activities में। Psychosocial impact बच्चे पर।
Congenital Anomalies
Associated cervical spine abnormalities जो surgical correction require करती हैं। Klippel-Feil syndrome जैसी conditions। Vertebral fusion या anomalies। Combined surgical approach जरूरी।
🔬 Pre-Operative Assessment (सर्जरी से पहले की तैयारी):
- Detailed Physical Examination: ROM measurement, muscle tightness assessment, craniofacial symmetry evaluation
- Imaging Studies: Cervical spine X-rays (AP और lateral) - vertebral anomalies rule out करने के लिए। MRI अगर neurological concerns हों। 3D CT scan अगर severe craniofacial asymmetry हो
- Hip Screening: Hip dysplasia (DDH) rule out - 20% association है। Hip ultrasound या X-ray जरूरी
- Vision Assessment: Ophthalmology consult - eye muscle imbalance check करना
- Anesthesia Clearance: Complete blood work, fitness for general anesthesia
- Parent Counseling: Realistic expectations, surgery details, post-op PT की importance समझाना
✂️ Surgical Procedures (सर्जरी के प्रकार):
1. Bipolar SCM Release
सबसे common procedure! SCM muscle के दोनों ends (sternal + clavicular origins और mastoid insertion) को release किया जाता है। यह most effective technique है। Z-plasty technique से scarring minimal होती है।
2. Unipolar SCM Release
केवल एक end (usually distal/mastoid end) को release किया जाता है। Mild contractures में adequate हो सकता है। Less invasive but कभी-कभी incomplete correction।
3. SCM Lengthening
Z-plasty या step-cut technique से muscle को lengthen किया जाता है। Muscle function preserve रहता है। Young children में preferred। Good functional outcomes।
4. Endoscopic Release
Minimally invasive technique। Small incisions through endoscope। Cosmetically better results। Less scarring। Recovery faster। Specialized equipment और expertise जरूरी।
5. Craniofacial Correction
Severe asymmetry cases में। Skull reshaping procedures। Helmet therapy post-surgery। Combine किया जाता है SCM release के साथ। Plastic surgeon collaboration।
6. Cervical Spine Surgery
अगर vertebral anomalies हों। Fusion procedures। Decompression if needed। Rare cases में। Spine surgeon involvement जरूरी।
🏥 Surgical Technique Details (विस्तृत प्रक्रिया):
📋 Step-by-Step Bipolar SCM Release:
- Step 1 - Positioning: बच्चे को supine position (पीठ के बल) लिटाया जाता है। Shoulder के नीचे small roll। Head को opposite side में rotate किया जाता है।
- Step 2 - Anesthesia: General anesthesia with endotracheal intubation। Muscle relaxation जरूरी है proper release के लिए।
- Step 3 - Skin Incision: 2-3 cm transverse incision supraclavicular area में (lower neck)। Skin crease में रखा जाता है - better cosmesis के लिए।
- Step 4 - Muscle Identification: SCM muscle के sternal और clavicular heads को carefully identify किया जाता है। Surrounding structures (carotid vessels, jugular vein) को protect करना।
- Step 5 - Distal Release: SCM को mastoid insertion से release किया जाता है। या muscle के lower third में Z-plasty। Complete release ensure करना।
- Step 6 - Proximal Release: Sternal और clavicular origins को release करना। Bipolar complete release।
- Step 7 - ROM Check: Intra-operative ROM check - full passive correction achieve हुआ या नहीं। Neck को all directions में freely move होना चाहिए।
- Step 8 - Hemostasis: Proper bleeding control। Drain placement अगर जरूरी हो (usually नहीं लगाते)।
- Step 9 - Closure: Layered closure - muscle, subcutaneous tissue, skin। Absorbable sutures use करते हैं। Subcuticular closure for better cosmesis।
- Step 10 - Dressing: Soft dressing apply करना। Cervical collar कभी-कभी 1-2 weeks के लिए।
⏱️ Surgery Duration & Hospital Stay:
🏥 Post-Operative Care (सर्जरी के बाद देखभाल):
📅 Immediate Post-Op (0-2 weeks):
- Pain Management: Oral pain medications - Paracetamol, Ibuprofen। Usually mild pain ही होता है
- Wound Care: Dressing dry रखना। Sutures 10-14 days में remove (या absorbable)। Scar massage बाद में
- Cervical Collar: कभी-कभी 1-2 weeks के लिए - overcorrection maintain करने के लिए
- Activity: Gentle neck movements encourage करें। कोई heavy lifting या jerky movements नहीं
- Infection Watch: Fever, redness, discharge - तुरंत doctor को inform करें
🔄 Early Recovery (2-6 weeks):
- PT Start करना: CRITICAL! 2 weeks बाद physiotherapy शुरू। Without PT, recurrence हो सकता है!
- Gentle Stretching: Opposite direction में gentle stretching। Scar tissue formation prevent करना
- ROM Exercises: All directions में neck movement। Gradually increase करना
- Positioning: Overcorrected position में ज्यादा time spend करना
- Weekly Follow-up: ROM progress monitor करना। Complications check करना
💪 Long-term Recovery (6 weeks - 6 months):
- Intensive PT: Daily exercises continue करना। Muscle strengthening। Balance training
- Full ROM Achievement: 3-6 months में full ROM expected। Persistent exercises जरूरी
- Scar Management: Massage, silicone sheets। Cosmetic outcome improve करने के लिए
- Activity Progression: Gradually normal activities resume करना। Sports clearance 3-4 months में
- Monitoring: Craniofacial symmetry improvement check करना। Photos document करना
⚠️ सबसे महत्वपूर्ण बात!
Post-operative physiotherapy ही surgery की success की KEY है! बिना PT के, muscle फिर से tight हो सकती है और recurrence हो सकता है। Daily exercises और regular PT sessions absolutely essential हैं।
⚠️ Possible Complications (संभावित जटिलताएं):
Recurrence (फिर से होना)
सबसे common complication - 5-15% cases में। कारण: inadequate PT, incomplete release, scar tissue formation। Prevention: intensive post-op PT!
Bleeding/Hematoma
Rare - <2% cases। Neck में swelling। Usually resolves spontaneously। Large hematoma को drain करना पड़ सकता है। Good surgical technique से prevent किया जा सकता है।
Infection
बहुत rare - <1% cases। Wound redness, fever, discharge। Antibiotics से treatment। Proper sterile technique से prevention। Clean wound care जरूरी।
Scarring
Visible scar neck में। Usually fades with time। Scar massage, silicone sheets help करते हैं। Z-plasty technique से minimize किया जाता है। Cosmetically acceptable।
Nerve Injury
Very rare complication। Accessory nerve (trapezius weakness) या facial nerve। Usually temporary। Careful surgical technique से avoid किया जाता है। Expert surgeon जरूरी।
Overcorrection
Temporary overcorrection deliberately किया जाता है। Usually resolves naturally। Persistent overcorrection rare। PT से manage किया जा सकता है।
💰 Surgery Cost (खर्च कितना होगा?):
💵 Approximate Cost Breakdown:
- Pre-operative Tests: ₹3,000 - 5,000 (X-rays, blood tests, ultrasound)
- Surgery Charges: ₹40,000 - 80,000 (surgeon fee, anesthesia, OT charges)
- Hospital Stay: ₹10,000 - 20,000 (1-2 days, room charges, nursing)
- Medications: ₹2,000 - 5,000 (antibiotics, pain medicines)
- Post-op PT: ₹500 - 1,500 per session × 20-30 sessions = ₹10,000 - 45,000
- Follow-up Visits: ₹500 - 1,000 per visit × 5-10 visits = ₹5,000 - 10,000
- Total Estimated Cost: ₹70,000 - 1,65,000
नोट: Cost hospital facilities, surgeon experience, और city पर depend करता है। Government hospitals में काफी कम cost हो सकती है। Insurance coverage check करें!
📊 Success Rates & Outcomes:
- Overall Success Rate: 90-95% excellent outcomes
- Complete ROM Achievement: 85-90% cases में full range of motion
- Cosmetic Improvement: Craniofacial asymmetry में significant improvement
- Recurrence Rate: 5-15% (mostly due to inadequate PT)
- Patient Satisfaction: >90% parents very satisfied
- Functional Outcomes: Normal neck function, no long-term disability
- Revision Surgery Rate: <5% cases में जरूरी
✅ Key Success Factors:
- Experienced Surgeon: Pediatric orthopedic surgeon का experience बहुत important
- Proper Patient Selection: Right timing और right indications
- Complete Release: Adequate surgical release - partial release ineffective
- Intensive Post-op PT: This is THE MOST IMPORTANT factor!
- Parent Compliance: Home exercises और follow-up में dedication
- Early Intervention: जितनी जल्दी surgery (if needed), उतना बेहतर
⚠️ Important:
Surgery is only necessary in 5-10% of cases. It's a LAST RESORT option when conservative treatment (PT, stretching) fails after 6-12 months. Dr. Gaurav Jain is an experienced pediatric orthopedic surgeon expert in torticollis surgery.
🎯 Surgical Indications (When is it necessary?):
Age > 12-18 Months
Child is over 12-18 months with persistent tightness. This is the ideal surgical age window as adequate conservative treatment trial has been completed by this time.
Failed Conservative Treatment
No significant improvement despite 6 months of intensive PT and stretching. Less than 30 degrees improvement in range of motion. Persistent SCM tightness.
Severe Contracture
Severe fibrosis and contracture in SCM muscle. Adequate ROM not achieved even with passive stretching. Muscle permanently shortened with fibrous tissue formation.
Craniofacial Asymmetry
Significant asymmetry developed in face and head. Progressive plagiocephaly (flat head). Uneven facial bone development. Increasing cosmetic concern.
Secondary Problems
Developing vision problems. Secondary cervical spine deformity. Shoulder girdle asymmetry. Functional limitations in daily activities. Psychosocial impact on child.
Congenital Anomalies
Associated cervical spine abnormalities requiring surgical correction. Conditions like Klippel-Feil syndrome. Vertebral fusion or anomalies. Combined surgical approach necessary.
🔬 Pre-Operative Assessment:
- Detailed Physical Examination: ROM measurement, muscle tightness assessment, craniofacial symmetry evaluation
- Imaging Studies: Cervical spine X-rays (AP and lateral) to rule out vertebral anomalies. MRI if neurological concerns. 3D CT scan if severe craniofacial asymmetry
- Hip Screening: Rule out hip dysplasia (DDH) - 20% association. Hip ultrasound or X-ray necessary
- Vision Assessment: Ophthalmology consult to check eye muscle imbalance
- Anesthesia Clearance: Complete blood work, fitness for general anesthesia
- Parent Counseling: Setting realistic expectations, surgery details, importance of post-op PT
✂️ Surgical Procedures (Types of Surgery):
1. Bipolar SCM Release
Most common procedure! Both ends of SCM muscle (sternal + clavicular origins and mastoid insertion) are released. This is the most effective technique. Z-plasty technique minimizes scarring.
2. Unipolar SCM Release
Only one end (usually distal/mastoid end) is released. May be adequate for mild contractures. Less invasive but sometimes incomplete correction.
3. SCM Lengthening
Muscle lengthened using Z-plasty or step-cut technique. Muscle function preserved. Preferred in young children. Good functional outcomes.
4. Endoscopic Release
Minimally invasive technique. Small incisions through endoscope. Cosmetically better results. Less scarring. Faster recovery. Requires specialized equipment and expertise.
5. Craniofacial Correction
For severe asymmetry cases. Skull reshaping procedures. Post-surgery helmet therapy. Combined with SCM release. Plastic surgeon collaboration.
6. Cervical Spine Surgery
If vertebral anomalies present. Fusion procedures. Decompression if needed. Rare cases. Spine surgeon involvement necessary.
🏥 Surgical Technique Details:
📋 Step-by-Step Bipolar SCM Release:
- Step 1 - Positioning: Child placed in supine position (on back). Small roll under shoulder. Head rotated to opposite side.
- Step 2 - Anesthesia: General anesthesia with endotracheal intubation. Muscle relaxation necessary for proper release.
- Step 3 - Skin Incision: 2-3 cm transverse incision in supraclavicular area (lower neck). Placed in skin crease for better cosmesis.
- Step 4 - Muscle Identification: Carefully identify sternal and clavicular heads of SCM. Protect surrounding structures (carotid vessels, jugular vein).
- Step 5 - Distal Release: Release SCM from mastoid insertion or Z-plasty in lower third of muscle. Ensure complete release.
- Step 6 - Proximal Release: Release sternal and clavicular origins. Complete bipolar release.
- Step 7 - ROM Check: Intra-operative ROM check - ensure full passive correction achieved. Neck should move freely in all directions.
- Step 8 - Hemostasis: Proper bleeding control. Drain placement if necessary (usually not required).
- Step 9 - Closure: Layered closure - muscle, subcutaneous tissue, skin. Use absorbable sutures. Subcuticular closure for better cosmesis.
- Step 10 - Dressing: Apply soft dressing. Cervical collar sometimes for 1-2 weeks.
⏱️ Surgery Duration & Hospital Stay:
🏥 Post-Operative Care:
📅 Immediate Post-Op (0-2 weeks):
- Pain Management: Oral pain medications - Paracetamol, Ibuprofen. Usually only mild pain
- Wound Care: Keep dressing dry. Suture removal in 10-14 days (or absorbable). Scar massage later
- Cervical Collar: Sometimes for 1-2 weeks to maintain overcorrection
- Activity: Encourage gentle neck movements. No heavy lifting or jerky movements
- Infection Watch: Fever, redness, discharge - inform doctor immediately
🔄 Early Recovery (2-6 weeks):
- Start PT: CRITICAL! Begin physiotherapy after 2 weeks. Without PT, recurrence possible!
- Gentle Stretching: Gentle stretching in opposite direction. Prevent scar tissue formation
- ROM Exercises: Neck movement in all directions. Gradually increase
- Positioning: Spend more time in overcorrected position
- Weekly Follow-up: Monitor ROM progress. Check for complications
💪 Long-term Recovery (6 weeks - 6 months):
- Intensive PT: Continue daily exercises. Muscle strengthening. Balance training
- Full ROM Achievement: Full ROM expected in 3-6 months. Persistent exercises necessary
- Scar Management: Massage, silicone sheets. Improve cosmetic outcome
- Activity Progression: Gradually resume normal activities. Sports clearance at 3-4 months
- Monitoring: Check craniofacial symmetry improvement. Document with photos
⚠️ Most Important Point!
Post-operative physiotherapy is THE KEY to surgical success! Without PT, muscle can become tight again and recurrence may occur. Daily exercises and regular PT sessions are absolutely essential.
⚠️ Possible Complications:
Recurrence
Most common complication - 5-15% of cases. Causes: inadequate PT, incomplete release, scar tissue formation. Prevention: intensive post-op PT!
Bleeding/Hematoma
Rare - <2% cases. Neck swelling. Usually resolves spontaneously. Large hematoma may need drainage. Prevented by good surgical technique.
Infection
Very rare - <1% cases. Wound redness, fever, discharge. Treatment with antibiotics. Prevention by proper sterile technique. Clean wound care necessary.
Scarring
Visible scar on neck. Usually fades with time. Scar massage, silicone sheets help. Minimized by Z-plasty technique. Cosmetically acceptable.
Nerve Injury
Very rare complication. Accessory nerve (trapezius weakness) or facial nerve. Usually temporary. Avoided by careful surgical technique. Expert surgeon necessary.
Overcorrection
Temporary overcorrection deliberately done. Usually resolves naturally. Persistent overcorrection rare. Managed with PT.
💰 Surgery Cost:
💵 Approximate Cost Breakdown:
- Pre-operative Tests: ₹3,000 - 5,000 (X-rays, blood tests, ultrasound)
- Surgery Charges: ₹40,000 - 80,000 (surgeon fee, anesthesia, OT charges)
- Hospital Stay: ₹10,000 - 20,000 (1-2 days, room charges, nursing)
- Medications: ₹2,000 - 5,000 (antibiotics, pain medicines)
- Post-op PT: ₹500 - 1,500 per session × 20-30 sessions = ₹10,000 - 45,000
- Follow-up Visits: ₹500 - 1,000 per visit × 5-10 visits = ₹5,000 - 10,000
- Total Estimated Cost: ₹70,000 - 1,65,000
Note: Cost depends on hospital facilities, surgeon experience, and city. Government hospitals may have significantly lower costs. Check insurance coverage!
📊 Success Rates & Outcomes:
- Overall Success Rate: 90-95% excellent outcomes
- Complete ROM Achievement: Full range of motion in 85-90% cases
- Cosmetic Improvement: Significant improvement in craniofacial asymmetry
- Recurrence Rate: 5-15% (mostly due to inadequate PT)
- Patient Satisfaction: >90% parents very satisfied
- Functional Outcomes: Normal neck function, no long-term disability
- Revision Surgery Rate: Necessary in <5% cases
✅ Key Success Factors:
- Experienced Surgeon: Pediatric orthopedic surgeon's experience very important
- Proper Patient Selection: Right timing and right indications
- Complete Release: Adequate surgical release - partial release ineffective
- Intensive Post-op PT: This is THE MOST IMPORTANT factor!
- Parent Compliance: Dedication in home exercises and follow-up
- Early Intervention: The earlier the surgery (if needed), the better
घर पर देखभाल और रोकथाम
Home Care & Prevention
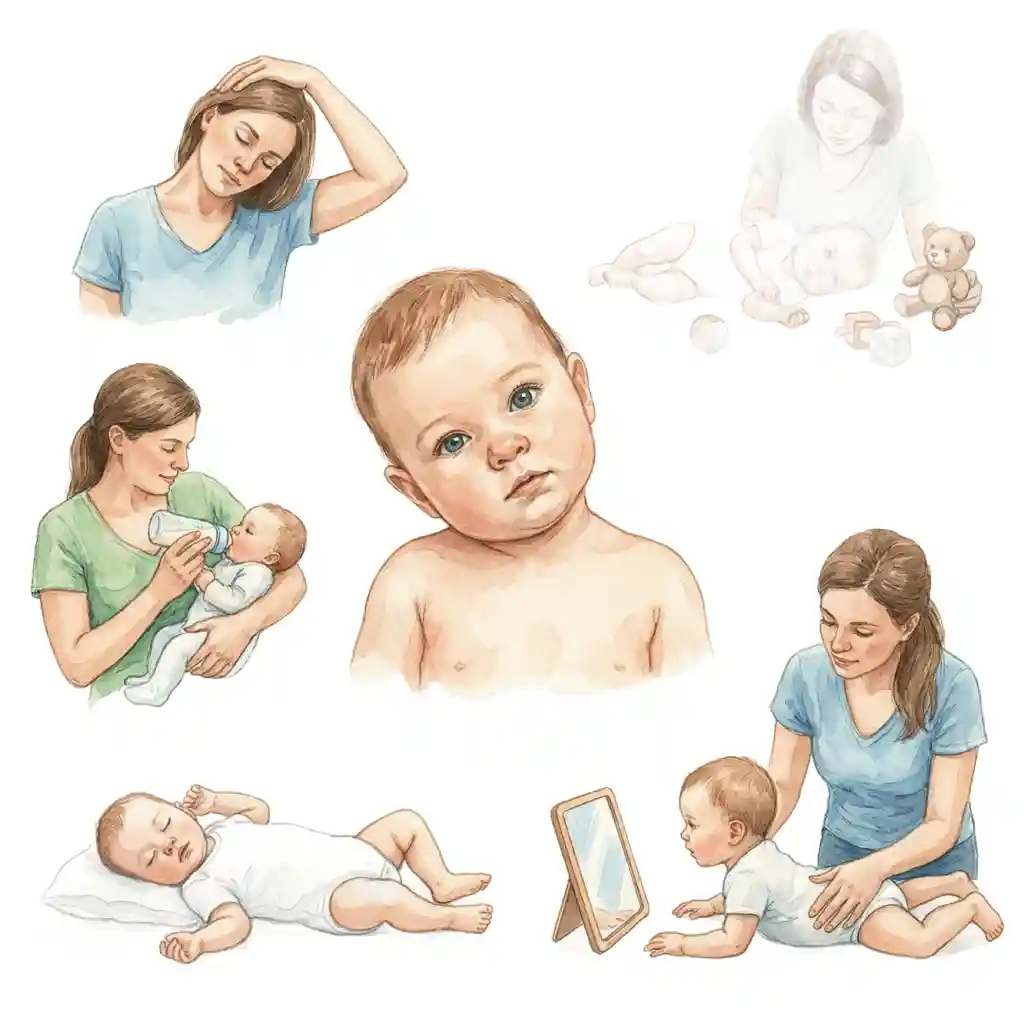
🏠 घर पर देखभाल के टिप्स:
Daily Stretching
Physiotherapist द्वारा सिखाई गई exercises रोज करें। दिन में 4-5 बार। Gentle और consistent रहें। कभी force न करें।
Positioning Strategy
Toys और interesting objects affected side पर रखें। बच्चे को naturally गर्दन घुमाने के लिए encourage करें।
Feeding Position
Opposite side से feed करें। दोनों तरफ से बराबर time दें। Bottle feeding में भी sides alternate करें।
Sleep Position
Head position regularly change करें। "Back to sleep" for safety but vary head turning। Flat head prevention!
Tummy Time
Supervised tummy time daily दें। Neck muscles strengthen होती हैं। Motor development में भी help करता है।
Visual Stimulation
Affected side से आंखों से follow करने के लिए encourage करें। Mirrors और colorful toys use करें।
🛡️ रोकथाम के उपाय:
- Good prenatal care: गर्भावस्था के दौरान proper care
- Vary baby's position: एक ही position में लंबे समय तक न रखें
- Limit car seat time: Car seat और carriers में limited time
- Encourage active movement: बच्चे को freely move करने दें
- Regular tummy time: Daily supervised tummy time
- Alternate sides: Feeding, holding, playing - सभी में sides alternate करें
⚠️ कब Doctor से Consult करें?
अगर आप notice करें कि बच्चे का सिर हमेशा एक तरफ झुका रहता है, गर्दन घुमाने में दिक्कत है, या गर्दन में गांठ महसूस होती है - तुरंत pediatric orthopedic surgeon से संपर्क करें!
🏠 Home Care Tips:
Daily Stretching
Perform exercises taught by physiotherapist daily. 4-5 times a day. Be gentle and consistent. Never force.
Positioning Strategy
Place toys and interesting objects on affected side. Encourage baby to naturally turn neck.
Feeding Position
Feed from opposite side. Give equal time to both sides. Alternate sides in bottle feeding too.
Sleep Position
Regularly change head position. "Back to sleep" for safety but vary head turning. Prevents flat head!
Tummy Time
Provide supervised tummy time daily. Strengthens neck muscles. Also helps motor development.
Visual Stimulation
Encourage visual tracking from affected side. Use mirrors and colorful toys.
🛡️ Prevention Measures:
- Good prenatal care: Proper care during pregnancy
- Vary baby's position: Don't keep in same position for long periods
- Limit car seat time: Limited time in car seats and carriers
- Encourage active movement: Let baby move freely
- Regular tummy time: Daily supervised tummy time
- Alternate sides: Alternate sides in feeding, holding, playing
⚠️ When to Consult Doctor?
If you notice your baby's head is always tilted to one side, difficulty turning neck, or feel a lump in the neck - contact a pediatric orthopedic surgeon immediately!
परिणाम और भविष्य
Prognosis & Outcomes
✅ Excellent Prognosis:
- Early treatment: जल्दी treatment शुरू करने पर outcomes बेहतरीन होते हैं
- High success rate: 90% cases physical therapy से completely resolve हो जाते हैं
- Normal development: Properly treated बच्चे normal development achieve करते हैं
- No long-term issues: Early treatment से कोई long-term problems नहीं होती
- Surgery success: अगर surgery जरूरी हो, तो भी success rate बहुत high है
🌟 महत्वपूर्ण संदेश:
Torticollis 100% treatable condition है! जल्दी diagnosis और proper treatment से लगभग सभी बच्चे completely normal neck movement achieve कर सकते हैं। Parents की active participation और consistency ही success की key है!
✅ Excellent Prognosis:
- Early treatment: Outcomes are excellent when treatment starts early
- High success rate: 90% of cases completely resolve with physical therapy
- Normal development: Properly treated children achieve normal development
- No long-term issues: Early treatment prevents any long-term problems
- Surgery success: Even when surgery is needed, success rate is very high
🌟 Important Message:
Torticollis is a 100% treatable condition! With early diagnosis and proper treatment, almost all children can achieve completely normal neck movement. Parent's active participation and consistency are the keys to success!
अक्सर पूछे जाने वाले सवाल (FAQ)
Frequently Asked Questions (FAQ)
Torticollis के बारे में सबसे common सवालों के जवाब यहां हैं। Category select करें या सभी देखें:
Here are answers to the most common questions about Torticollis. Select a category or view all:
क्या torticollis serious है? / Is torticollis serious?
NO, torticollis is NOT serious in most cases! यह एक very treatable condition है। 90% cases physical therapy से completely ठीक हो जाते हैं। जल्दी treatment शुरू करने पर excellent outcomes मिलते हैं। कोई permanent damage नहीं होता। बस regular exercises और follow-up जरूरी है।
बिना surgery के ठीक होगा? / Will it heal without surgery?
YES! 90% cases बिना surgery के ठीक हो जाते हैं! Physical therapy और stretching exercises ही सबसे effective treatment है। Surgery केवल 5-10% cases में जरूरी होती है जब conservative treatment fail हो। Daily exercises और proper positioning से excellent results मिलते हैं। Early start करना जरूरी!
कितने समय में ठीक होता है? / How long to heal?
3-6 महीने में significant improvement! Mild cases: 2-3 months। Moderate cases: 4-6 months। Severe cases: 6-12 months या more। 95% cases 1 year तक resolved हो जाते हैं। Daily exercises consistency बहुत important है। जितनी जल्दी treatment start हो, उतना fast recovery!
घर पर क्या करें? / What to do at home?
Daily home exercises बहुत जरूरी! (1) Stretching exercises 4-5 times daily (2) Toys affected side पर रखें (3) Feeding opposite side से (4) Sleep position vary करें (5) Supervised tummy time (6) Visual stimulation। PT sessions में सीखे हुए exercises regularly करें। Consistency ही key है। Never force stretches!
Physical therapy कब शुरू करें? / When to start PT?
जितनी जल्दी हो सके, उतना बेहतर! Ideal: 3-6 months की age तक start करें। Early intervention से best results मिलते हैं। देरी से शुरू करने पर भी effective है लेकिन समय ज्यादा लग सकता है। Diagnosis होते ही PT referral लें। Trained pediatric physiotherapist जरूरी। Regular sessions + home program essential!
क्या congenital torticollis बार-बार होता है? / Does it recur?
NO! Properly treated torticollis recur नहीं होता। एक बार completely resolve हो जाने के बाद permanent correction मिलता है। Follow-up exercises और maintenance जरूरी हो सकती हैं। अगर new torticollis develop हो तो वह different cause से होगा। Prevention के लिए proper positioning maintain करें। Relapse बहुत rare है!
Botox injection कब जरूरी है? / When is Botox needed?
Selected cases में जब PT response नहीं मिलता। Age > 6-9 months और persistent tightness। Severe spasticity में। PT को easier बनाने के लिए। Temporary effect - 3-6 months। PT के साथ combined therapy। Adult spasmodic torticollis में भी। Not first-line treatment - trial of PT first!
Face asymmetry ठीक होगी? / Will facial asymmetry resolve?
YES, usually resolves with treatment! Early treatment (< 6 months age): face asymmetry पूरी तरह normal हो जाती है। Later treatment: significant improvement होता है but complete symmetry नहीं मिल सकती। Skull molding devices भी help कर सकते हैं। जितनी जल्दी treatment, उतना बेहतर face symmetry!
Feeding में दिक्कत हो तो? / If feeding difficulty?
Opposite side से feed करने की कोशिश करें। Position vary करें। Support pillows use करें। Patience रखें - time लग सकता है। Lactation consultant से help लें। Bottle feeding में भी same principle। Never force! Gradual progress होगा। PT exercises से feeding भी easier हो जाती है।
Surgery कब जरूरी है? / When is surgery required?
केवल 5-10% cases में जरूरी! Indications: (1) Age > 12 months और persistent tightness (2) Failed conservative treatment (6+ months PT) (3) Severe contracture (4) Significant craniofacial asymmetry। Surgery: SCM muscle release। Post-surgery intensive PT essential। Success rate बहुत high। Last resort option!
Genetic है क्या? / Is it genetic?
NO, torticollis generally genetic नहीं है। यह inherited condition नहीं है। Birth trauma या positioning से होता है। Family history से connection नहीं है। अगले बच्चे में होने की chances normal population जितनी ही हैं। Prevention: proper positioning during pregnancy और delivery। Genetic counseling जरूरी नहीं!
Sleep position कैसी रखें? / What sleep position?
Always "Back to Sleep" for safety! लेकिन head position vary करें। Alternate left/right head turning। Rolled towel से gentle positioning। Never force! Flat head prevention important। Tummy time during awake supervised periods। Sleep environment safe रखें। Positioning devices only if recommended by doctor।
Hip dysplasia भी check करें? / Check for hip dysplasia?
YES! Hip screening जरूरी है। 20% torticollis babies को hip dysplasia (DDH) भी होता है। Association well-documented। Hip ultrasound करवाएं। Early detection से treatment आसान। Routine screening recommended। Both conditions साथ treat किए जा सकते हैं। Regular follow-up जरूरी!
Normal development होगी? / Will development be normal?
YES! Properly treated children develop normally। Torticollis से intellectual development affected नहीं होता। Motor milestones slightly delayed हो सकते हैं but catch up होता है। Speech, cognition normal। Social development normal। With proper treatment - completely normal future। No long-term limitations!
Exercises कितनी बार करें? / How often exercises?
दिन में 4-5 बार, हर बार 10-15 stretches। Each stretch 10-15 seconds hold। Gentle और controlled movements। Never force या cause pain। Consistency daily basis पर जरूरी। Diaper changes, feeding times के साथ combine करें। PT sessions: weekly या bi-weekly। Home program ही main treatment है!
TOT collar कैसे काम करता है? / How does TOT collar work?
Head को correct position में maintain करता है। Tubular Orthosis for Torticollis (TOT)। Gentle stretching provide करता है। Several hours daily wear किया जाता है। PT के साथ combined use। Not for all cases - moderate to severe में। Doctor prescription जरूरी। Regular monitoring essential!
Success rate क्या है? / What's the success rate?
90% success rate with PT! Early treatment (< 6 months): 95%+ success। Later treatment: 80-90% success। Surgery cases: 95%+ excellent outcomes। Overall prognosis EXCELLENT! Proper compliance key है। Almost all children achieve normal neck function। Long-term outcomes very good!
Diagnosis कैसे confirm होता है? / How is it diagnosed?
Physical examination + Ultrasound। Doctor neck mobility और muscle tightness check करते हैं। Palpable lump in SCM। Ultrasound confirms muscle involvement। X-rays: spine abnormality rule out। Hip screening essential। Eye examination। Early diagnosis usually clinical - tests confirm!
Treatment cost कितनी है? / What's the treatment cost?
PT sessions: ₹500-1,500 per session। Weekly sessions × 3-6 months। Initial assessment: ₹1,000-2,000। Ultrasound: ₹1,500-3,000। Surgery (if needed): ₹50,000-1,50,000। Home exercises free - parent-performed। Overall affordable compared to other conditions। Early treatment = lower overall cost!
पूरी तरह ठीक हो सकता है? / Can it be completely cured?
YES! Torticollis 100% curable है! Early diagnosis और proper treatment से complete cure। Normal neck movement। Normal appearance। No long-term problems। 90%+ children completely recover। Excellent prognosis। Success depends on: early start, consistency, proper technique। भविष्य bilkul normal होता है!
Surgery painful होती है? / Is surgery painful?
Surgery के दौरान NO pain - general anesthesia! Post-op pain: MILD ही होता है। 2-3 days तक discomfort। Pain medicines से easily manage होता है। Children surprisingly well tolerate करते हैं। 1 week में pain minimal। Compared to other surgeries, यह relatively less painful है।
Surgery में कितना time लगता है? / Surgery duration?
45-90 minutes typically! Simple unipolar release: 30-45 min। Bipolar release: 60-90 min। Endoscopic: 45-60 min। Combined procedures: longer। Depends on: severity, technique, surgeon experience। OT में total time (prep + surgery + recovery): 2-3 hours। Safe और quick procedure!
Hospital में कितने दिन रहना पड़ेगा? / Hospital stay duration?
Usually 1-2 days ही! Day of surgery: observation। Next day: discharge if all well। Some cases: same day discharge possible (6-8 hours observation)। Total stay: 24-48 hours। Uncomplicated cases में early discharge। Home care instructions दिए जाते हैं। Follow-up OPD में।
Scar कितनी बड़ी होगी? / How big is the scar?
Small scar - 2-3 cm केवल! Lower neck में एक small horizontal line। Skin crease में hidden। 6-12 months में significantly fades। Scar massage, silicone sheets से और improve। Endoscopic: even smaller scars। Cosmetically acceptable। Most parents very satisfied। Better than persistent torticollis!
Surgery के बाद फिर से हो सकता है? / Can it recur after surgery?
5-15% cases में recurrence possible। Main cause: INADEQUATE POST-OP PT! बिना proper PT के, scar tissue contracture बन सकता है। Prevention: intensive daily PT, stretching, positioning। Early recurrence detection जरूरी। Mild recurrence: PT से manage। Severe recurrence: revision surgery may be needed। Proper PT = lowest recurrence risk!
Surgery के बाद PT कब शुरू करें? / When to start PT after surgery?
2 weeks बाद formal PT start! First 2 weeks: wound healing। Gentle ROM exercises start कर सकते हैं। After suture removal (10-14 days): intensive PT begin। Daily sessions + home program। 3-6 months तक continue। यह CRITICAL है! PT ही surgery को successful बनाता है। Skipping PT = high recurrence risk!
Surgery के risks क्या हैं? / What are surgery risks?
Overall VERY SAFE surgery! Risks: (1) Recurrence 5-15% - preventable with PT (2) Infection <1% (3) Bleeding <2% (4) Nerve injury very rare (5) Scarring - usually acceptable (6) Anesthesia risks - minimal। Serious complications बहुत rare। Expert surgeon = lower risks। Benefits far outweigh risks in indicated cases!
Surgery की सही age क्या है? / Best age for surgery?
12-18 months = ideal window! Younger than 12 months: PT trial incomplete। Older than 18 months: OK but craniofacial changes ज्यादा। Sweet spot: 15-18 months। But surgery की age flexibility है - even 2-3 years में good results। Timing depends on: severity, PT response, family readiness। Discuss with surgeon!
Surgery के बाद normal activities कब? / When normal activities after surgery?
Gradual return to activities! Week 1-2: gentle activities, avoid vigorous play। Week 3-4: increase activity level। 6-8 weeks: most normal activities। 3-4 months: full sports clearance। Swimming: after complete wound healing (3-4 weeks)। School: 1-2 weeks बाद। Each child different - follow surgeon's advice!
Surgery success rate क्या है? / Surgery success rate?
90-95% EXCELLENT success rate! Full ROM achievement: 85-90%। Good to excellent results: 90-95%। Parent satisfaction: >90%। Cosmetic improvement: significant। Functional outcomes: normal। Success factors: (1) Experienced surgeon (2) Complete release (3) Post-op PT compliance। Dr. Gaurav Jain के साथ excellent outcomes expected!
Bipolar vs Unipolar release - difference? / कौन सी surgery बेहतर?
Bipolar usually preferred! Bipolar: both ends release - more complete correction, higher success। Unipolar: single end release - less invasive, mild cases में OK। Choice depends on: severity, age, previous treatments। Surgeon decides best option। Bipolar में slightly longer surgery but better long-term results। Most cases में bipolar recommended!
Anesthesia safe है? / Is anesthesia safe for infants?
YES! Modern pediatric anesthesia बहुत safe है! Experienced pediatric anesthesiologist। Continuous monitoring during surgery। Short anesthesia duration (1-2 hours)। Risks minimal। Thousands of similar surgeries safely performed। Pre-operative assessment करते हैं। Emergency backup available। Benefits of surgery far exceed anesthesia risks। Don't worry - very safe!
Discharge के बाद घर पर क्या care करें? / Home care after discharge?
Home care tips: (1) Pain medicines regularly initially (2) Wound को dry रखें, no water 1 week (3) Gentle neck movements encourage करें (4) Avoid heavy lifting/jerky movements (5) Watch for fever, discharge (6) Follow positioning advice (7) Start gentle stretches as advised (8) Keep follow-up appointments (9) Document ROM progress। Instructions sheet दी जाती है!
Follow-up visits कितनी बार? / How many follow-ups?
Regular follow-ups जरूरी! Schedule: Week 1-2: suture removal, wound check। Week 4-6: ROM assessment, PT progress। Month 3: improvement check। Month 6: final assessment। Then yearly check-ups। Total: 5-10 visits first year। Photos document करना। ROM measurements। Early problem detection। Adjustments in PT program। Most important first 6 months!
Total treatment cost कितनी होगी? / Total cost including surgery?
Total: ₹70,000 - 1,65,000 approximately। Breakdown: Pre-op tests ₹3-5k, Surgery ₹40-80k, Hospital ₹10-20k, Medicines ₹2-5k, Post-op PT ₹10-45k, Follow-ups ₹5-10k। Government hospitals: much lower। Private hospitals: higher end। Insurance may cover। Dr. Gaurav Jain provides transparent pricing। Worth it for permanent correction!
📞 Dr. Gaurav Jain से Consult करें - Indore!
📞 Consult Dr. Gaurav Jain - Indore!
Torticollis Expert | Physical Therapy | Stretching | Surgery Torticollis Expert | Physical Therapy | Stretching | Surgery
📞 अभी Call करें 📞 Call Now