
Osteogenesis Imperfecta
Osteogenesis Imperfecta
Brittle Bone Disease - Expert Treatment & Care
Brittle Bone Disease - Expert Treatment & Care
Osteogenesis Imperfecta क्या है?
What is Osteogenesis Imperfecta?
Osteogenesis Imperfecta (OI) एक genetic disorder है जिसे "Brittle Bone Disease" भी कहते हैं। Collagen defect के कारण bones कमजोर होती हैं और आसानी से टूट जाती हैं। Birth से ही condition present होती है। NO CURE - लेकिन treatment से quality of life improve होती है।
🎯 Key Facts!
Brittle Bone Disease! 1:15,000 to 1:20,000 births। Genetic mutation causes। Collagen Type 1 defect। Range: mild से severe। Multiple fractures common! Treatment improves outcomes। Lifelong condition!
📊 Key Statistics:
जन्मों में
सबसे common
जीवनकाल में
आनुवंशिक
🧬 What Happens?
Collagen Type 1 में defect - bones की main building block।
Causes: COL1A1 or COL1A2 gene mutations। कभी-कभी spontaneous mutation। Autosomal dominant या recessive।
Result: Weak bones → frequent fractures। Abnormal bone structure। Low bone mass। Blue sclera। Hearing loss।
🔑 Important: Genetic disorder! Birth से present। Can be inherited या new mutation। Affects bone formation throughout life।
⚠️ Common Misconceptions:
- Myth: OI बढ़ती है। Fact: Genetic - birth से present! Severity varies।
- Myth: सभी OI children wheelchair में। Fact: Many walk independently!
- Myth: Cure possible। Fact: Lifelong condition - but treatable!
- Myth: सभी severe। Fact: Wide spectrum - mild से severe!
Osteogenesis Imperfecta (OI) is genetic disorder known as "Brittle Bone Disease". Collagen defect causes weak bones that break easily. Present from birth. NO CURE - but treatment improves quality of life.
🎯 Key Facts!
Most common inherited bone disorder! 1:15,000 births. Collagen Type 1 defect. Multiple types. Frequent fractures. Early intervention crucial!
📊 Stats:
OI के प्रकार (Types)
Types of OI
🎯 8 Main Types Based on Severity!
Type I (Mildest) | Type II (Lethal) | Type III (Severe) | Type IV (Moderate) | Types V-VIII (Rare)
📋 OI Types Detailed:
1. Type I OI (50%)
MILDEST AND MOST COMMON! Blue sclera। Few fractures (mostly childhood)। Normal या near-normal height। Hearing loss possible। Good prognosis! Independent life। Mild bone deformity। Teeth may be normal या brittle (DI)।
2. Type II OI
MOST SEVERE - LETHAL! Usually stillborn या die shortly after birth। Extreme bone fragility। Multiple fractures at birth। Severe deformities। Small chest। Respiratory failure। Prenatal diagnosis possible! Genetic counseling important।
3. Type III OI
SEVERE - PROGRESSIVE! Multiple fractures from birth। Short stature (very short)। Severe bone deformities। Blue/grey sclera। Dentinogenesis imperfecta common। Wheelchair dependent often। Respiratory issues। Hearing loss। Require intensive care।
4. Type IV OI
MODERATE SEVERITY! White या light blue sclera। Moderate bone deformities। Short stature (mild-moderate)। Variable fractures। Many walk independently! Dentinogenesis imperfecta common। Bowing of bones। Better prognosis than Type III।
5. Types V-VIII OI
RARE TYPES! Recently identified। Different genetic mutations। Type V: Calcified interosseous membrane। Type VI: Specific bone pathology। Types VII-VIII: Recessive inheritance। Research ongoing! Similar management to Types III-IV।
✅ Type I vs Type III Comparison:
Type I: Mild। Blue sclera। Few fractures। Normal height possible। Independent। Type III: Severe। Very short। Many fractures। Deformities। Wheelchair often। Both need specialized care!
🧬 Genetics & Inheritance:
Types I, IV: Autosomal dominant - 50% chance। Type II: Usually new mutation या autosomal recessive। Types VII-VIII: Autosomal recessive - 25% chance। Genetic testing available! Counseling recommended for families। Prenatal diagnosis possible।
🎯 8 Types - Mild to Lethal!
Type I (Mild) | Type II (Lethal) | Type III (Severe) | Type IV (Moderate)
Main Types:
Type I
Mildest. Blue sclera. Few fractures. Normal height. Good prognosis.
Type II
Most severe. Lethal. Multiple fractures at birth. Prenatal diagnosis.
Type III
Severe. Very short. Multiple deformities. Wheelchair often.
Type IV
Moderate. Variable fractures. Many walk. Better outcomes.
लक्षण (Symptoms)
Symptoms & Signs
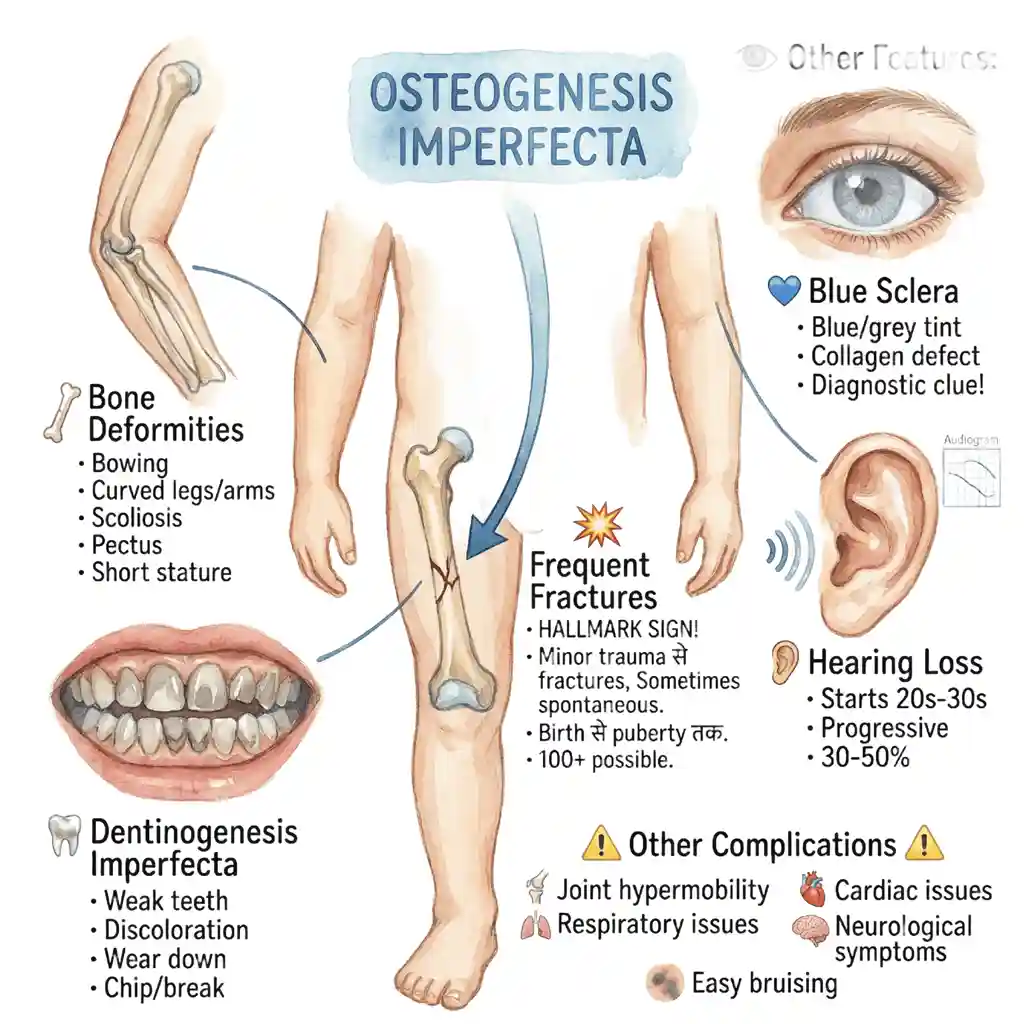
🚨 Main Features of OI!
Frequent Fractures | Blue Sclera | Bone Deformities | Short Stature | Hearing Loss
🦴 Skeletal Symptoms:
Frequent Fractures
HALLMARK SIGN! Minor trauma से fractures। Sometimes spontaneous fractures। Birth से लेकर puberty तक most common। Long bones (femur, tibia)। Decrease after puberty। 100+ fractures possible in lifetime। Proper handling crucial!
Bone Deformities
Bowing of long bones। Curved legs/arms। Scoliosis (spine curvature)। Pectus deformity (chest)। Progressive with repeated fractures। Growth plate damage। Short stature common। Surgery may be needed।
Short Stature
Variable by type। Type I: normal या slightly short। Type III: very short (severe)। Type IV: mild-moderate short। Due to: Bone deformities। Compression fractures। Growth plate issues। Adult height affected।
Dentinogenesis Imperfecta
Weak teeth (DI)। Grey/brown discoloration। Wear down easily। Chip/break easily। Common in Types III, IV। Dental care important। Crowns/veneers needed। Prevent infections।
👁️ Other Features:
💙 Blue Sclera (Common!)
Blue या grey tint to whites of eyes। Due to thin sclera। Collagen defect causes। Most prominent in Type I। May fade with age। NOT harmful। Diagnostic clue!
👂 Hearing Loss (30-50%)
Usually starts in 20s-30s। Conductive या sensorineural। Progressive। Small ear bone (stapes) affected। Treatment: Hearing aids। Surgery (stapedectomy)। Regular audiometry। Early detection important!
⚠️ Other Complications:
- Joint hypermobility - Loose joints। Ligament laxity। Dislocations।
- Respiratory issues - Small chest। Rib fractures। Restrictive lung disease।
- Cardiac issues - Valve problems (rare)। Aortic dilation।
- Basilar invagination - Skull base abnormality। Neurological symptoms।
- Easy bruising - Fragile blood vessels। Bleeding tendency।
🔍 Diagnosis:
Clinical features - Blue sclera + fractures। X-rays - Osteopenia, thin cortices। Bone density (DXA) - Low BMD। Genetic testing - Confirms mutation। Prenatal: Ultrasound, amniocentesis। Biochemical: Collagen testing। Early diagnosis = better management!
🚨 Main Features!
Fractures | Blue Sclera | Deformities | Short Stature | Hearing Loss
Key Symptoms:
Frequent Fractures
Hallmark! Minor trauma. Birth to puberty. 100+ possible.
Bone Deformities
Bowing. Scoliosis. Progressive. Surgery needed.
Blue Sclera
Common Type I. Diagnostic clue. Thin sclera.
Hearing Loss
30-50%. Starts 20s-30s. Hearing aids help.
Treatment & Management
Treatment & Management
🏥 Multidisciplinary Approach!
Medications + Surgery + PT + Nutrition + Support!
NO CURE - but comprehensive management reduces fractures, improves mobility, quality of life!
🎯 Main Treatment Options:
Bisphosphonates
GOLD STANDARD! Pamidronate/Zoledronic acid। Increases bone density। Reduces fractures (30-50%)। IV infusion। Start early! Side effects: Flu-like symptoms। Lifelong treatment। Regular monitoring। Dr. Gaurav Jain provides!
Orthopedic Surgery
Rodding surgery! Intramedullary rods in long bones। Prevents deformities। Fassier-Duval rods grow with child। Scoliosis surgery। Fracture fixation। Optimal timing crucial। Multiple surgeries often needed। Dr. Gaurav Jain specializes!
Physiotherapy
Essential component! Strengthening exercises। Range of motion। Mobility training। GENTLE! Avoid high-impact। Swimming excellent। Hydrotherapy। Prevents contractures। Build muscle strength। Lifelong need।
Nutrition & Supplements
Adequate calcium (1000-1500mg/day)। Vitamin D (800-1000 IU)। Balanced diet। Maintain healthy weight। NOT too heavy। Protein important। Avoid smoking/alcohol। Nutrition counseling। Monitor growth।
Assistive Devices
Wheelchairs for severe cases। Walkers। Braces/orthotics। Lightweight materials! Proper cushioning। Prevent fractures। Adaptive equipment। Home modifications। Promote independence।
Pain Management
Analgesics as needed। Fracture pain significant! NSAIDs। Nerve pain medications। Physical therapy। Psychological support। Avoid opioid dependence। Acute vs chronic pain।
✅ Fracture Management:
Immobilization: Minimal casting time। Light casts। Early mobilization! Prevent muscle wasting। Healing: Normal healing time। Monitor alignment। Prevention: Avoid falls। Safe environment। Protective gear। Gentle handling। Education for family/school!
⚠️ Treatment Goals:
- Reduce fractures - Primary goal। Bisphosphonates help।
- Improve mobility - PT, surgery। Assistive devices।
- Maximize independence - Adaptive strategies। Life skills।
- Prevent complications - Scoliosis, deformities। Early intervention।
- Optimize quality of life - Holistic approach। Psychological support।
🔬 Emerging Therapies:
Research ongoing! Gene therapy trials। New medications (Denosumab, Teriparatide)। Stem cell research। Future promising! Clinical trials available। Experimental treatments। Hope for better outcomes। Stay informed!
🏥 Comprehensive Management!
Medications + Surgery + PT + Nutrition!
NO CURE - but treatment improves outcomes significantly!
Main Treatments:
Bisphosphonates
Gold standard! Reduces fractures 30-50%. IV infusion. Lifelong.
Rodding Surgery
Intramedullary rods. Fassier-Duval. Prevents deformities.
Physiotherapy
Gentle strengthening. Swimming. Prevents contractures.
Nutrition
Calcium 1000-1500mg. Vitamin D. Healthy weight.
अक्सर पूछे जाने वाले सवाल (FAQ)
Frequently Asked Questions (FAQ)
Osteogenesis Imperfecta क्या है? / What is OI?
Genetic disorder - "Brittle Bone Disease"! Collagen Type 1 defect। Bones weak और easily break। Birth से present। 8 types। 1:15,000 births। NO CURE - but treatable! Bisphosphonates, surgery, PT help। Lifelong management needed!
Cure possible? / क्या ठीक हो सकता?
NO CURE! Genetic disorder - permanent। BUT - treatment greatly improves quality of life! Bisphosphonates reduce fractures 30-50%। Surgery prevents deformities। PT improves mobility। Many lead active lives। Gene therapy research ongoing!
OI के types? / Types of OI?
8 main types! Type I (50%) - Mildest, blue sclera। Type II - Lethal। Type III - Severe, very short। Type IV - Moderate। Types V-VIII - Rare। Severity varies widely। Type determines prognosis। Genetic testing identifies type!
Best treatment? / सबसे अच्छा इलाज?
Bisphosphonates = GOLD STANDARD! Pamidronate/Zoledronic acid। Increases bone density। Reduces fractures 30-50%। Plus: Rodding surgery, PT, nutrition, pain management। Multidisciplinary approach best। Start treatment early। Lifelong management। Dr. Gaurav Jain provides comprehensive care!
Bisphosphonates कैसे काम करते? / How do bisphosphonates work?
Slow bone breakdown (resorption)। Increase bone density। Strengthen bones। IV infusion - every 3-6 months। Side effects: Flu-like symptoms 1-2 days। Safe long-term। Monitor with DXA scans। Reduces fractures significantly। Start in infancy/childhood। Continue lifelong!
Rodding surgery क्या है? / What is rodding surgery?
Intramedullary rods inserted into long bones। Prevents bowing/deformities। Fassier-Duval rods - GROW with child! Done for severe/recurrent fractures। Femur, tibia most common। Multiple surgeries often needed। Improves mobility। Reduces fracture risk। Dr. Gaurav Jain performs!
Genetic? / आनुवंशिक है?
YES - genetic disorder! COL1A1 या COL1A2 gene mutations। 90% inherited। 10% new (spontaneous) mutations। Autosomal dominant (Types I, IV) - 50% chance to children। Autosomal recessive (Types II, III, VII-VIII) - 25% chance। Genetic testing available। Counseling important। Prenatal diagnosis possible!
Blue sclera क्यों? / Why blue sclera?
Thin sclera (eye white)। Collagen defect causes। Underlying choroid shows through - appears blue/grey। Most prominent in Type I। May fade with age। NOT harmful। Important diagnostic sign। NOT all OI patients have blue sclera!
Fracture होने पर? / When fracture happens?
Immobilize immediately। Gentle handling। Light cast/splint। Minimal immobilization time। Early mobilization important! Healing time normal। Pain management। X-ray to confirm। Monitor alignment। PT after healing। Prevent muscle wasting। Document fractures। Pattern helps diagnosis।
क्या चल पाएंगे? / Will child walk?
Depends on type! Type I: YES - almost all walk independently। Type IV: Most walk - some need aids। Type III: Many wheelchair-dependent। But with treatment, rodding, PT - MANY achieve mobility! Early intervention crucial। Bisphosphonates help। Surgery improves outcomes। Don't lose hope!
Height कितनी होगी? / How tall?
Type I: Normal या slightly short (160+ cm possible)। Type III: Very short (adult 90-120 cm)। Type IV: Moderately short (130-160 cm)। Depends on: Fractures, deformities, treatment। Growth hormone NOT effective। Rodding may help। Accept और adapt!
Fractures कब तक? / Till what age fractures?
Most common: Birth to puberty। Decrease after puberty (hormones help)। Type I: Significant decrease after teens। Types III, IV: May continue in adulthood। Women: Increase after menopause। Bisphosphonates reduce at all ages। Safe environment always important!
Teeth की problem? / Teeth problems?
Dentinogenesis Imperfecta (DI) in 50%। Teeth grey/brown। Weak और chip easily। Wear down। Common in Types III, IV। Treatment: Good oral hygiene। Crowns/veneers। Gentle brushing। Avoid hard foods। Regular dental care। Preventive approach। Cosmetic options available।
Mental development? / मानसिक विकास?
NORMAL intelligence! OI affects bones, NOT brain। Cognitive development normal। Children can excel academically। Some may have learning challenges due to absences (fractures/surgery)। Social development important। Psychological support helpful। Many OI adults successful professionals!
Hearing loss? / सुनने में कमी?
30-50% develop hearing loss। Usually starts 20s-30s। Progressive। Stapes (ear bone) affected। Conductive या sensorineural। Treatment: Hearing aids effective। Surgery (stapedectomy) option। Regular audiometry important। Early detection key। Not all patients affected!
Exercise allowed? / व्यायाम कर सकते?
YES - but gentle! Swimming - BEST exercise। Hydrotherapy। Cycling। Yoga (modified)। AVOID: Contact sports। High-impact। Jumping। Benefits: Muscle strength। Bone health। Mobility। Consult PT। Individualized program। Balance safety + activity!
Treatment cost? / खर्चा कितना?
Varies widely! Bisphosphonates: ₹15,000-30,000/infusion। Rodding surgery: ₹2,00,000-5,00,000+। PT, medications, assistive devices additional। Lifelong expenses। Government schemes available। Insurance coverage। NGO support। Prioritize bisphosphonates + critical surgeries। Dr. Gaurav Jain helps plan affordable care!
Pregnancy में? / During pregnancy?
Women with OI CAN have children। Risks: Fractures during pregnancy। Pelvic issues। C-section often needed। Anesthesia considerations। Stop bisphosphonates before conception। Genetic counseling important। 50% chance (Type I, IV)। Prenatal diagnosis available। High-risk pregnancy। Specialized care essential!
Home care tips? / घर पर देखभाल?
(1) Safe environment - Padded corners। No stairs। (2) Gentle handling - Support head/body। (3) Calcium/Vitamin D daily। (4) Regular PT exercises। (5) Avoid falls - Non-slip floors। (6) Proper lifting। (7) Adaptive equipment। (8) School education। (9) Emotional support। (10) Regular doctor visits। Love + care + safety!
Life expectancy? / जीवन प्रत्याशा?
Type I, IV: NORMAL lifespan! Type II: Lethal (usually at birth)। Type III: Reduced - but many live to 50s-60s with care। Complications: Respiratory, cardiovascular। With modern treatment - outcomes improving! Bisphosphonates, surgery help। Many OI adults lead fulfilling lives! Quality of life good!
📞 Dr. Gaurav Jain से Consult करें - Indore!
📞 Consult Dr. Gaurav Jain - Indore!
Osteogenesis Imperfecta Expert | Bisphosphonate Therapy | Rodding Surgery Osteogenesis Imperfecta Expert | Bisphosphonate Therapy | Rodding Surgery
📞 अभी Call करें 📞 Call Now