Juvenile Rheumatoid Arthritis (JIA)
बच्चों में गठिया - पूरी जानकारी और इलाज
Juvenile Rheumatoid Arthritis (JIA)
Complete information and treatment for Childhood Arthritis
Juvenile Rheumatoid Arthritis (JIA) क्या है? What is Juvenile Rheumatoid Arthritis (JIA)?
Juvenile Idiopathic Arthritis (JIA) - जिसे पहले Juvenile Rheumatoid Arthritis (JRA) कहा जाता था - बच्चों में होने वाली chronic arthritis है। "Juvenile" means <16 years age। "Idiopathic" means unknown cause। "Arthritis" means joint inflammation।
यह एक autoimmune disease है जहां body की immune system गलती से अपने ही joints को attack करती है, सोचकर कि ये foreign हैं। Result: joint inflammation, pain, swelling, stiffness। यह chronic condition है - लंबे समय तक चलती है, कभी-कभी lifetime।
NOT just "adult arthritis in children"! JIA अलग है adult rheumatoid arthritis से - different patterns, different prognosis, different treatment response। कई बच्चे adult age तक पहुंचते-पहुंचते remission में चले जाते हैं (disease inactive हो जाती है)।
कब Doctor से मिलना चाहिए?
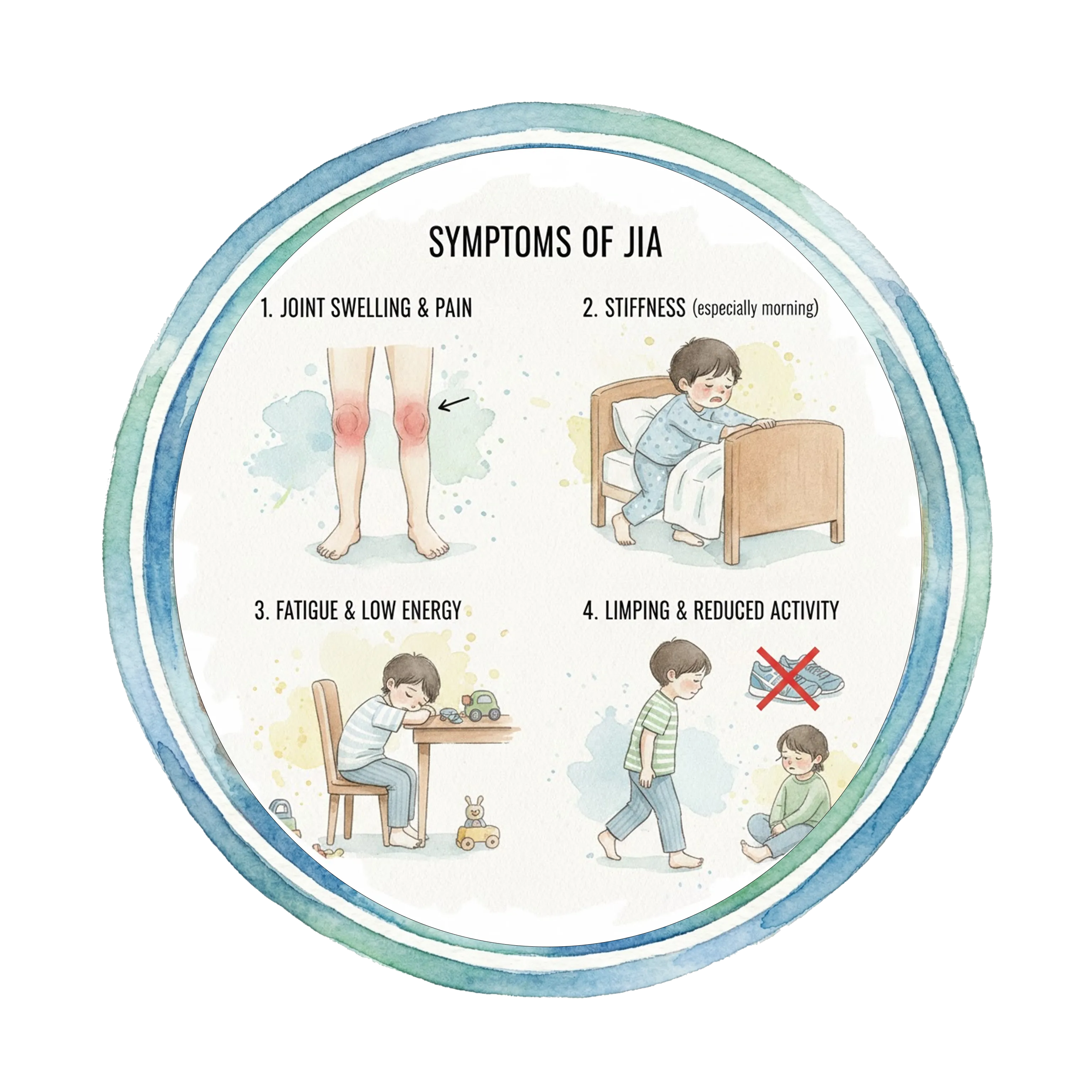
• Joint pain - 6 weeks से ज्यादा lasting
• Joint swelling - visible या palpable
• Morning stiffness - बच्चा सुबह stiff, "ठीक से चल नहीं पाता"
• Limping - खासकर सुबह
• Joint warmth - joints गर्म महसूस होते हैं
• Difficulty with daily activities - दौड़ना, खेलना difficult
• Refusing to use arm या leg
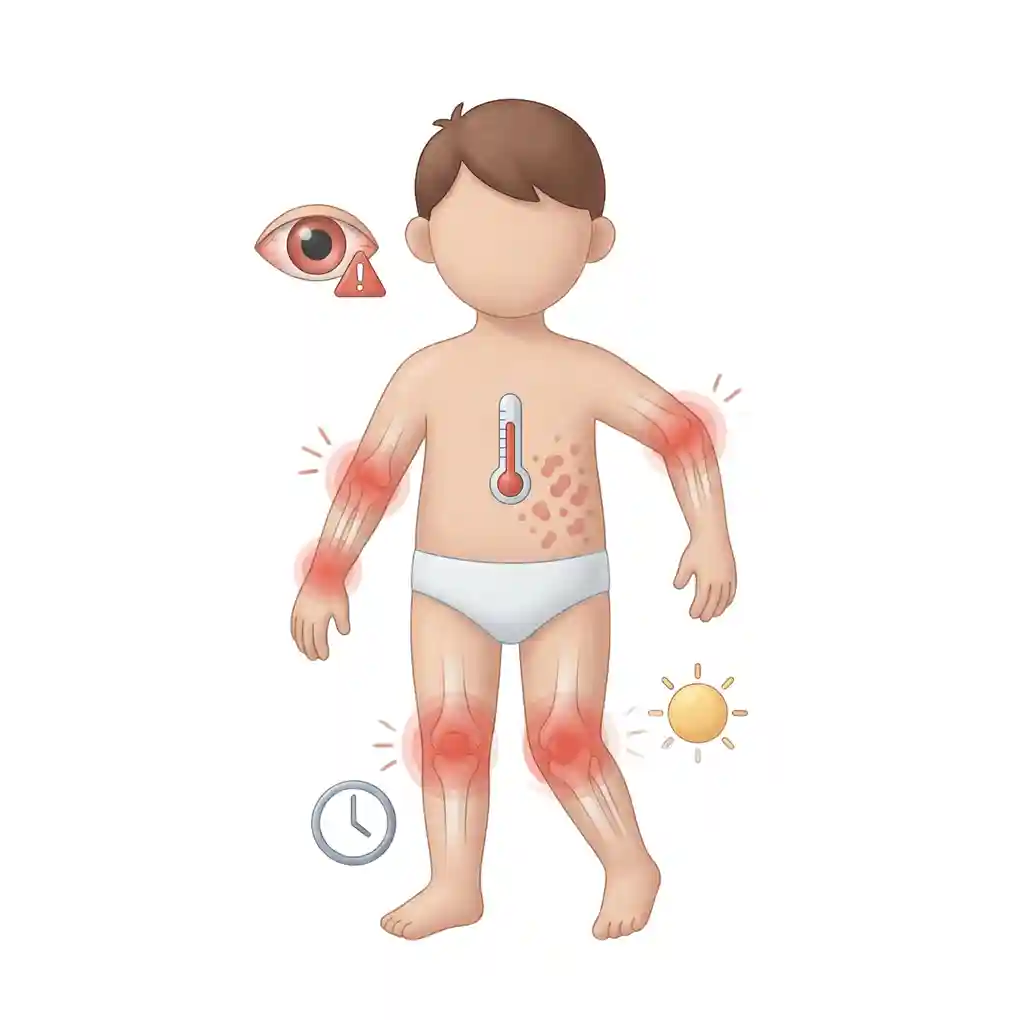
• Persistent fever - साथ में rash
• Eye redness या pain (uveitis - serious complication)
• Growth problems - एक limb दूसरे से छोटा
• Fatigue, tiredness - excessive for age
• Multiple joints involved
⏰ URGENT if: Eye pain/redness, high fever with rash, severe pain, joint very hot and red।
Juvenile Idiopathic Arthritis (JIA) - previously called Juvenile Rheumatoid Arthritis (JRA) - is chronic arthritis occurring in children. "Juvenile" means <16 years age. "Idiopathic" means unknown cause. "Arthritis" means joint inflammation.
It's an autoimmune disease where body's immune system mistakenly attacks own joints, thinking they're foreign. Result: joint inflammation, pain, swelling, stiffness. This is chronic condition - lasts long time, sometimes lifetime.
NOT just "adult arthritis in children"! JIA is different from adult rheumatoid arthritis - different patterns, different prognosis, different treatment response. Many children go into remission (disease becomes inactive) by adult age.
When to See Doctor?
• Joint pain - lasting >6 weeks
• Joint swelling - visible or palpable
• Morning stiffness - child stiff in morning, "can't walk properly"
• Limping - especially in morning
• Joint warmth - joints feel hot
• Difficulty with daily activities - running, playing difficult
• Refusing to use arm or leg
• Persistent fever - with rash
• Eye redness or pain (uveitis - serious complication)
• Growth problems - one limb shorter than other
• Fatigue, tiredness - excessive for age
• Multiple joints involved
⏰ URGENT if: Eye pain/redness, high fever with rash, severe pain, joint very hot and red.
JIA के Types Types of JIA
Oligoarticular JIA
सबसे common type (50%):
Definition: 4 या fewer joints involved - पहले 6 months में।
Typically affects:
• Large joints - knees, ankles, wrists
• Usually asymmetric (एक side ज्यादा)
• Girls > Boys (4:1)
• Age: 2-4 years common
Types:
• Persistent: 4 या fewer joints पूरे disease course में
• Extended: >4 joints बाद में involve होते हैं
Key concern - UVEITIS:
• Eye inflammation - 20-30% cases
• Often silent - no symptoms initially
• Can cause blindness if untreated
• Regular eye exams ESSENTIAL (हर 3-4 months)
Prognosis: Generally best। Many achieve remission। But uveitis risk remains।
Polyarticular JIA
5+ joints involved:
Two subtypes:
1. RF-negative (Rheumatoid Factor negative):
• 20-30% of JIA cases
• Girls > Boys
• Any age
• Small और large joints both
• Symmetric usually
• Moderate severity
2. RF-positive (Rheumatoid Factor positive):
• 5-10% of JIA - less common
• Older children (adolescence)
• Girls >> Boys
• Most similar to adult RA
• Aggressive disease
• High joint damage risk
• Worst prognosis
Joints affected:
• Hands, wrists (common)
• Knees, ankles
• Neck, jaw
• Symmetric pattern
Impact: Significant disability possible if untreated। Early aggressive treatment needed।
Systemic JIA (Still's Disease)
Most severe form (10%):
Triad of features:
1. Fever:
• High spiking fever - 39-40°C
• Daily spikes - usually evening
• Returns to normal between spikes
• Lasts weeks
2. Rash:
• Salmon-pink color
• Flat या slightly raised
• Trunk, extremities
• Comes and goes - especially with fever
• Evanescent (disappears quickly)
3. Arthritis:
• May appear later (weeks to months after fever)
• Any joints
• Can be severe
Other features:
• Hepatosplenomegaly (liver, spleen enlarged)
• Lymph node swelling
• Serositis (heart, lung lining inflammation)
Equal boys और girls।
Serious complication - MAS:
• Macrophage Activation Syndrome
• Life-threatening
• High fever, bleeding, organ failure
• Medical emergency
Prognosis: Variable। कुछ remission, कुछ chronic arthritis develop।
Enthesitis-Related Arthritis (ERA)
Affects entheses + joints:
Enthesis: Point where tendon/ligament attaches to bone।
Features:
• Boys >> Girls
• Older children (>8 years)
• Lower extremity arthritis - hips, knees, ankles
• Asymmetric
• Enthesitis - heel pain (Achilles), knee pain (patellar tendon)
• Back pain - sacroiliac joints
Associated with:
• HLA-B27 positive (genetic marker)
• Family history of ankylosing spondylitis
• Inflammatory bowel disease sometimes
Eye involvement:
• Acute uveitis (different from oligoarticular)
• Painful, red eye
• Sudden onset
Concern: May progress to ankylosing spondylitis in adulthood - spine stiffness।
Psoriatic Arthritis
Arthritis + psoriasis:
Criteria (need arthritis +1):
• Psoriasis in child
• OR Family history of psoriasis
• OR Dactylitis (sausage fingers/toes)
• OR Nail pitting
Note: Arthritis often appears BEFORE skin psoriasis!
Pattern:
• Can affect any joints
• Often asymmetric
• Small joints of hands/feet common
• Dactylitis - whole digit swollen
Nail changes:
• Pitting (small dents)
• Separation from nail bed
• Discoloration
Girls slightly > Boys।
Course: Variable। Can be mild या severe।
Undifferentiated Arthritis
Doesn't fit any category:
• Arthritis present
• But doesn't meet criteria for above types
• OR meets criteria for >1 type
Over time may:
• Evolve into specific type
• OR remain undifferentiated
Treatment: Based on severity और pattern।
Oligoarticular JIA
Most common type (50%):
Definition: 4 or fewer joints involved - in first 6 months.
Typically affects:
• Large joints - knees, ankles, wrists
• Usually asymmetric (one side more)
• Girls > Boys (4:1)
• Age: 2-4 years common
Types:
• Persistent: 4 or fewer joints throughout disease course
• Extended: >4 joints involved later
Key concern - UVEITIS:
• Eye inflammation - 20-30% cases
• Often silent - no symptoms initially
• Can cause blindness if untreated
• Regular eye exams ESSENTIAL (every 3-4 months)
Prognosis: Generally best. Many achieve remission. But uveitis risk remains.
Polyarticular JIA
5+ joints involved:
Two subtypes:
1. RF-negative (Rheumatoid Factor negative):
• 20-30% of JIA cases
• Girls > Boys
• Any age
• Both small and large joints
• Usually symmetric
• Moderate severity
2. RF-positive (Rheumatoid Factor positive):
• 5-10% of JIA - less common
• Older children (adolescence)
• Girls >> Boys
• Most similar to adult RA
• Aggressive disease
• High joint damage risk
• Worst prognosis
Joints affected:
• Hands, wrists (common)
• Knees, ankles
• Neck, jaw
• Symmetric pattern
Impact: Significant disability possible if untreated. Early aggressive treatment needed.
Systemic JIA (Still's Disease)
Most severe form (10%):
Triad of features:
1. Fever:
• High spiking fever - 39-40°C
• Daily spikes - usually evening
• Returns to normal between spikes
• Lasts weeks
2. Rash:
• Salmon-pink color
• Flat or slightly raised
• Trunk, extremities
• Comes and goes - especially with fever
• Evanescent (disappears quickly)
3. Arthritis:
• May appear later (weeks to months after fever)
• Any joints
• Can be severe
Other features:
• Hepatosplenomegaly (liver, spleen enlarged)
• Lymph node swelling
• Serositis (heart, lung lining inflammation)
Equal boys and girls.
Serious complication - MAS:
• Macrophage Activation Syndrome
• Life-threatening
• High fever, bleeding, organ failure
• Medical emergency
Prognosis: Variable. Some remission, some develop chronic arthritis.
Enthesitis-Related Arthritis (ERA)
Affects entheses + joints:
Enthesis: Point where tendon/ligament attaches to bone.
Features:
• Boys >> Girls
• Older children (>8 years)
• Lower extremity arthritis - hips, knees, ankles
• Asymmetric
• Enthesitis - heel pain (Achilles), knee pain (patellar tendon)
• Back pain - sacroiliac joints
Associated with:
• HLA-B27 positive (genetic marker)
• Family history of ankylosing spondylitis
• Inflammatory bowel disease sometimes
Eye involvement:
• Acute uveitis (different from oligoarticular)
• Painful, red eye
• Sudden onset
Concern: May progress to ankylosing spondylitis in adulthood - spine stiffness.
Psoriatic Arthritis
Arthritis + psoriasis:
Criteria (need arthritis +1):
• Psoriasis in child
• OR Family history of psoriasis
• OR Dactylitis (sausage fingers/toes)
• OR Nail pitting
Note: Arthritis often appears BEFORE skin psoriasis!
Pattern:
• Can affect any joints
• Often asymmetric
• Small joints of hands/feet common
• Dactylitis - whole digit swollen
Nail changes:
• Pitting (small dents)
• Separation from nail bed
• Discoloration
Girls slightly > Boys.
Course: Variable. Can be mild or severe.
Undifferentiated Arthritis
Doesn't fit any category:
• Arthritis present
• But doesn't meet criteria for above types
• OR meets criteria for >1 type
Over time may:
• Evolve into specific type
• OR remain undifferentiated
Treatment: Based on severity and pattern.
Diagnosis कैसे होता है? How is it Diagnosed?
JIA का diagnosis clinical है - कोई single test नहीं जो confirm करे। Diagnosis एक combination है: history, physical examination, blood tests, imaging, और exclusion of other causes।
Clinical Criteria
Definition of JIA: Arthritis in ≥1 joint for ≥6 weeks। Onset <16 years। Other causes excluded। Arthritis means: Joint swelling OR limited range of motion + pain/tenderness।
Blood Tests
NO test confirms JIA but helpful: CBC: Anemia, high WBC/platelets। ESR, CRP: Inflammation markers - elevated। RF (Rheumatoid Factor): Usually negative in children (only 5-10% positive - polyarticular RF+ type)। ANA (Antinuclear Antibody): Positive 40-50% - higher uveitis risk। HLA-B27: For ERA type। Other: Rule out infection, malignancy।
Imaging
X-rays: Early - often normal। Later - joint space narrowing, erosions, growth abnormalities। Ultrasound: Detect synovitis (joint lining inflammation), effusion। MRI: Most sensitive - early changes, cartilage damage। Expensive, not routine।
Eye Examination
MANDATORY - slit lamp exam: By ophthalmologist। Screen for uveitis - especially oligoarticular, ANA+ patients। Frequency: Every 3 months if high risk। Every 6 months if moderate risk। Lifetime screening needed!
Differential Diagnosis
Must exclude: Septic arthritis (infection), Reactive arthritis (post-infection), Lyme disease, Leukemia/malignancy, Inflammatory bowel disease-related arthritis, Systemic lupus erythematosus (SLE), Other rheumatic diseases।
JIA diagnosis is clinical - no single test confirms it. Diagnosis is combination of: history, physical examination, blood tests, imaging, and exclusion of other causes.
Clinical Criteria
Definition of JIA: Arthritis in ≥1 joint for ≥6 weeks. Onset <16 years. Other causes excluded. Arthritis means: Joint swelling OR limited range of motion + pain/tenderness.
Blood Tests
NO test confirms JIA but helpful: CBC: Anemia, high WBC/platelets. ESR, CRP: Inflammation markers - elevated. RF (Rheumatoid Factor): Usually negative in children (only 5-10% positive - polyarticular RF+ type). ANA (Antinuclear Antibody): Positive 40-50% - higher uveitis risk. HLA-B27: For ERA type. Other: Rule out infection, malignancy.
Imaging
X-rays: Early - often normal. Later - joint space narrowing, erosions, growth abnormalities. Ultrasound: Detect synovitis (joint lining inflammation), effusion. MRI: Most sensitive - early changes, cartilage damage. Expensive, not routine.
Eye Examination
MANDATORY - slit lamp exam: By ophthalmologist. Screen for uveitis - especially oligoarticular, ANA+ patients. Frequency: Every 3 months if high risk. Every 6 months if moderate risk. Lifetime screening needed!
Differential Diagnosis
Must exclude: Septic arthritis (infection), Reactive arthritis (post-infection), Lyme disease, Leukemia/malignancy, Inflammatory bowel disease-related arthritis, Systemic lupus erythematosus (SLE), Other rheumatic diseases.
Treatment - Medical और Surgical Treatment - Medical and Surgical
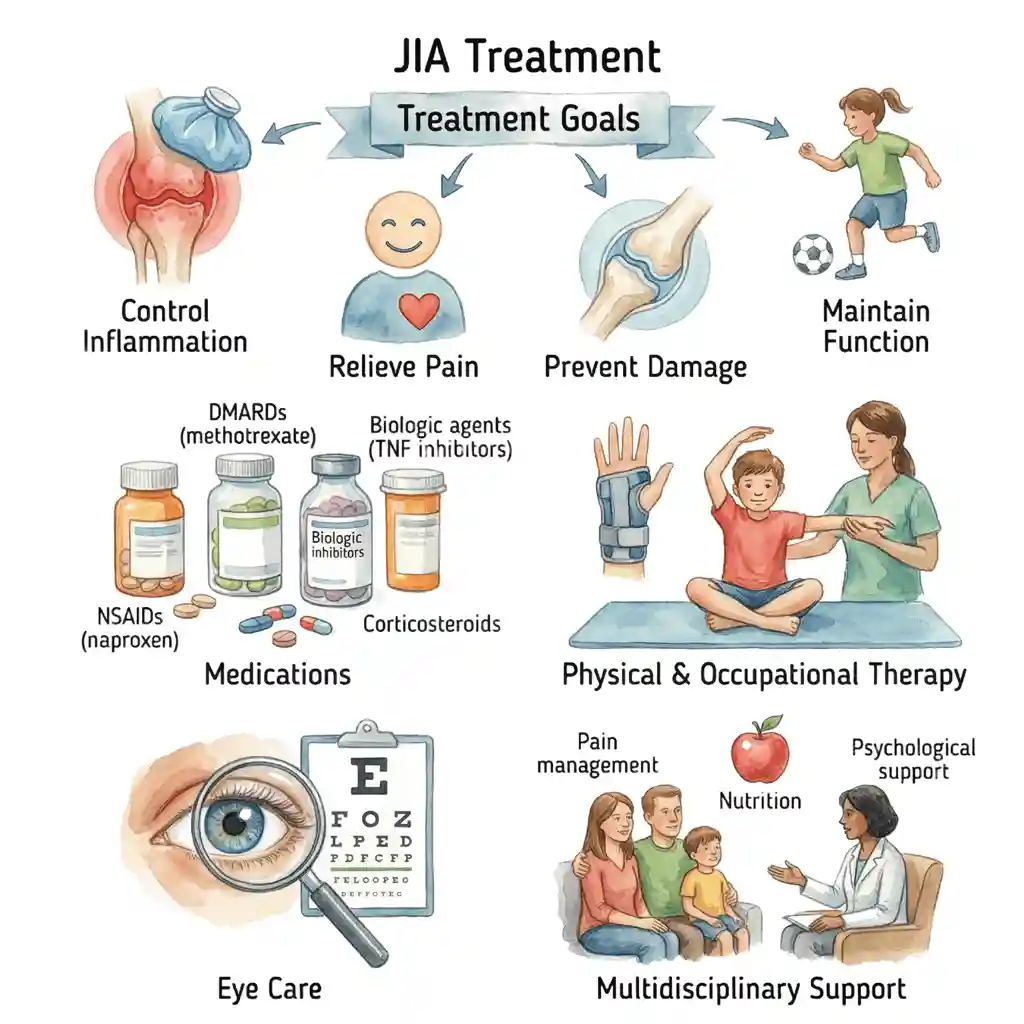
Treatment Goals
Primary goals: (1) Control inflammation - stop joint damage, (2) Relieve pain, (3) Preserve joint function, (4) Prevent complications - especially uveitis, (5) Maintain normal growth and development, (6) Optimize quality of life, (7) Achieve remission if possible।
Early aggressive treatment is KEY! "Window of opportunity" - early treatment prevents permanent damage।
MEDICAL TREATMENT
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
First-line for mild disease:
Common NSAIDs:
• Naproxen - most common
• Ibuprofen
• Indomethacin
• Meloxicam
How they work: Reduce inflammation और pain। Block COX enzyme।
Benefits:
• Quick symptom relief - days to weeks
• Safe for long-term use in children
• Oral - easy to take
Limitations:
• Don't prevent joint damage
• Symptomatic relief only
• Not enough for moderate-severe disease
Side effects:
• GI upset - stomach pain, nausea
• Rare - GI bleeding, kidney problems
• Take with food
Role: Adjunct therapy। Used WITH disease-modifying drugs।
DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
Cornerstone of JIA treatment:
METHOTREXATE - Gold Standard:
• Most commonly used DMARD
• Weekly dosing - oral या subcutaneous injection
• Takes 6-12 weeks to work - patience needed!
How it works: Suppresses immune system। Reduces inflammation। Prevents joint damage।
Effectiveness: 60-70% children improve significantly।
Monitoring:
• Blood tests every 4-8 weeks - liver, blood counts
• Folic acid supplement - reduce side effects
Side effects:
• Nausea (common) - anti-nausea meds help
• Mouth sores
• Hair thinning (rare)
• Liver enzyme elevation (monitor)
• Infection risk (mild increase)
Other DMARDs (less common):
• Sulfasalazine - especially ERA
• Leflunomide - alternative to MTX
• Hydroxychloroquine - mild cases
Key message: Methotrexate is SAFE और EFFECTIVE in children। Decades of data। Benefits >> risks।
Biologic Agents (Biologics)
Revolutionary treatment!
When used:
• Inadequate response to methotrexate
• Moderate-severe disease
• Systemic JIA
• Polyarticular RF+
Types:
1. TNF Inhibitors (most common):
• Etanercept (Enbrel): Subcutaneous, twice weekly। Most studied in children।
• Adalimumab (Humira): Subcutaneous, every 2 weeks।
• Infliximab (Remicade): IV infusion, every 8 weeks।
How they work: Block TNF-alpha - key inflammatory protein।
Effectiveness: 70-80% achieve significant improvement। Dramatic results often।
2. IL-6 Inhibitors:
• Tocilizumab (Actemra): Especially effective for systemic JIA। IV infusion।
3. IL-1 Inhibitors:
• Anakinra, Canakinumab: Systemic JIA।
4. Other:
• Abatacept (T-cell costimulation blocker)
• Rituximab (rare, severe cases)
Side effects:
• Injection site reactions
• Increased infection risk - screen for TB first
• Rare - serious infections
• Avoid live vaccines
Monitoring:
• TB screening before starting
• Watch for infections
• Regular follow-ups
Cost: Expensive - ₹50,000-2,00,000/month। Insurance coverage important।
Game-changer: Biologics transformed JIA treatment। Remission achievable in many।
Corticosteroids (Steroids)
Powerful anti-inflammatory:
Uses:
1. Intra-articular (Joint) Injections:
• Inject steroid directly into inflamed joint
• Quick relief - within days
• Lasts months
• Excellent for oligoarticular JIA - few joints
• Can repeat
• Minimal systemic side effects
• Preferred over oral steroids when possible
2. Systemic (Oral/IV) Steroids:
• Severe systemic JIA
• Bridging therapy - while waiting for DMARDs to work
• Disease flares
• Uveitis
Forms:
• Prednisone/Prednisolone - oral
• Methylprednisolone - IV pulse (severe cases)
Effectiveness: Very effective। Quick symptom control।
Side effects (long-term oral use):
• Growth suppression - MAJOR concern in children
• Weight gain - moon face, central obesity
• Bone loss - osteoporosis
• Infection risk
• Glucose intolerance
• Cataracts
• Cushingoid appearance
Goal: MINIMIZE oral steroid use!
• Use lowest dose, shortest duration
• Taper gradually
• Joint injections preferred
• Transition to steroid-sparing agents (MTX, biologics) ASAP
Never stop abruptly - adrenal suppression।
Physical और Occupational Therapy
Essential component of treatment!
Physical Therapy:
• Range of motion exercises - prevent stiffness
• Strengthening - support joints
• Stretching - maintain flexibility
• Hydrotherapy - pool exercises, gentle
• Pain management techniques
Occupational Therapy:
• Fine motor activities - hand function
• Daily living skills - dressing, eating
• Splints - rest joints, prevent deformity
• Joint protection techniques
• Adaptive equipment if needed
Goals:
• Maintain joint function
• Prevent contractures
• Maximize independence
• Return to normal activities
Frequency: Regular sessions - 2-3 times/week initially। Then home program।
Important: Exercise during remission too - prevent deconditioning।
Uveitis Treatment
Separate from joint treatment:
By Ophthalmologist:
• Topical steroids - eye drops
• Methotrexate - systemic
• Biologics - if resistant (Adalimumab approved)
• Mydriatic drops - prevent adhesions
Close monitoring: Can be sight-threatening। Aggressive treatment needed।
Often persists even when arthritis controlled! Lifelong screening needed।
SURGICAL TREATMENT
Surgery - When Needed?
Surgery is last resort in JIA। Modern medical treatment very effective - surgery much less common now than before biologics era। But still needed in some cases।
Synovectomy
Remove inflamed joint lining:
Indications:
• Persistent synovitis in single joint
• Despite medical treatment
• Risk of joint damage
• Pain affecting function
Procedure:
• Arthroscopic (keyhole) - preferred
• Remove inflamed synovium
• Knee most common
Outcomes:
• Pain relief
• Improved function
• May delay joint damage
• Not curative - can recur
Rare now - medical treatment usually controls।
Limb Length Correction
For leg length discrepancy:
Cause: Chronic arthritis में - knee inflammation → overgrowth of that leg। OR undergrowth if very severe।
Significant discrepancy (>2-3 cm):
• Epiphysiodesis - stop growth of longer leg
• Limb lengthening - rare, complex
• Timing critical
Goal: Equal leg lengths at skeletal maturity।
Soft Tissue Releases
For contractures:
When joints get stuck:
• Flexion contractures - can't fully straighten
• Limited range of motion
• Affecting function
Procedures:
• Tendon lengthening
• Capsule release
• Joint manipulation
Post-op: Aggressive PT essential।
Joint Replacement (Arthroplasty)
For severe joint damage:
When:
• End-stage arthritis
• Severe pain
• Major functional limitation
• Failed medical treatment
• Skeletal maturity (usually wait till adult)
Joints:
• Hip - most common
• Knee
• Rarely - shoulder, ankle
Challenge in JIA:
• Young age - implants don't last forever
• May need revision surgeries later
• Try to delay as long as possible
Outcomes:
• Excellent pain relief
• Improved function
• Better quality of life
• Can return to many activities
Rare now - early aggressive medical treatment prevents this।
Eye Surgery
For uveitis complications:
Procedures:
• Cataract surgery - if cataract develops
• Glaucoma surgery - if high eye pressure
• Adhesion release - if iris stuck
By ophthalmologist: Specialized care needed।
TMJ (Jaw) Surgery
If jaw involved:
TMJ arthritis:
• Micrognathia (small jaw)
• Limited mouth opening
• Eating difficulties
Treatments:
• Distraction osteogenesis - lengthen jaw
• Joint replacement - severe cases
• Orthodontics
Complex: Multidisciplinary - orthodontist, maxillofacial surgeon।
Modern JIA Treatment - Success Story!
20-30 years ago: Many JIA children → wheelchair, severe disability, joint replacements।
TODAY with modern treatment:
• 50-70% achieve remission या near-remission
• 70-80% lead normal lives - school, sports, work
• Joint damage rare if treated early
• Surgery much less common
• Quality of life excellent
Key to success:
✅ Early diagnosis
✅ Aggressive treatment from start
✅ Regular monitoring
✅ Medication compliance
✅ Team approach - rheumatologist, ophthalmologist, PT, OT
✅ Family support
The message is HOPE! JIA is manageable। Children CAN thrive।
Treatment Goals
Primary goals: (1) Control inflammation - stop joint damage, (2) Relieve pain, (3) Preserve joint function, (4) Prevent complications - especially uveitis, (5) Maintain normal growth and development, (6) Optimize quality of life, (7) Achieve remission if possible.
Early aggressive treatment is KEY! "Window of opportunity" - early treatment prevents permanent damage.
MEDICAL TREATMENT
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
First-line for mild disease:
Common NSAIDs:
• Naproxen - most common
• Ibuprofen
• Indomethacin
• Meloxicam
How they work: Reduce inflammation and pain. Block COX enzyme.
Benefits:
• Quick symptom relief - days to weeks
• Safe for long-term use in children
• Oral - easy to take
Limitations:
• Don't prevent joint damage
• Symptomatic relief only
• Not enough for moderate-severe disease
Side effects:
• GI upset - stomach pain, nausea
• Rare - GI bleeding, kidney problems
• Take with food
Role: Adjunct therapy. Used WITH disease-modifying drugs.
DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
Cornerstone of JIA treatment:
METHOTREXATE - Gold Standard:
• Most commonly used DMARD
• Weekly dosing - oral or subcutaneous injection
• Takes 6-12 weeks to work - patience needed!
How it works: Suppresses immune system. Reduces inflammation. Prevents joint damage.
Effectiveness: 60-70% children improve significantly.
Monitoring:
• Blood tests every 4-8 weeks - liver, blood counts
• Folic acid supplement - reduce side effects
Side effects:
• Nausea (common) - anti-nausea meds help
• Mouth sores
• Hair thinning (rare)
• Liver enzyme elevation (monitor)
• Infection risk (mild increase)
Other DMARDs (less common):
• Sulfasalazine - especially ERA
• Leflunomide - alternative to MTX
• Hydroxychloroquine - mild cases
Key message: Methotrexate is SAFE and EFFECTIVE in children. Decades of data. Benefits >> risks.
Biologic Agents (Biologics)
Revolutionary treatment!
When used:
• Inadequate response to methotrexate
• Moderate-severe disease
• Systemic JIA
• Polyarticular RF+
Types:
1. TNF Inhibitors (most common):
• Etanercept (Enbrel): Subcutaneous, twice weekly. Most studied in children.
• Adalimumab (Humira): Subcutaneous, every 2 weeks.
• Infliximab (Remicade): IV infusion, every 8 weeks.
How they work: Block TNF-alpha - key inflammatory protein.
Effectiveness: 70-80% achieve significant improvement. Dramatic results often.
2. IL-6 Inhibitors:
• Tocilizumab (Actemra): Especially effective for systemic JIA. IV infusion.
3. IL-1 Inhibitors:
• Anakinra, Canakinumab: Systemic JIA.
4. Other:
• Abatacept (T-cell costimulation blocker)
• Rituximab (rare, severe cases)
Side effects:
• Injection site reactions
• Increased infection risk - screen for TB first
• Rare - serious infections
• Avoid live vaccines
Monitoring:
• TB screening before starting
• Watch for infections
• Regular follow-ups
Cost: Expensive - ₹50,000-2,00,000/month. Insurance coverage important.
Game-changer: Biologics transformed JIA treatment. Remission achievable in many.
Corticosteroids (Steroids)
Powerful anti-inflammatory:
Uses:
1. Intra-articular (Joint) Injections:
• Inject steroid directly into inflamed joint
• Quick relief - within days
• Lasts months
• Excellent for oligoarticular JIA - few joints
• Can repeat
• Minimal systemic side effects
• Preferred over oral steroids when possible
2. Systemic (Oral/IV) Steroids:
• Severe systemic JIA
• Bridging therapy - while waiting for DMARDs to work
• Disease flares
• Uveitis
Forms:
• Prednisone/Prednisolone - oral
• Methylprednisolone - IV pulse (severe cases)
Effectiveness: Very effective. Quick symptom control.
Side effects (long-term oral use):
• Growth suppression - MAJOR concern in children
• Weight gain - moon face, central obesity
• Bone loss - osteoporosis
• Infection risk
• Glucose intolerance
• Cataracts
• Cushingoid appearance
Goal: MINIMIZE oral steroid use!
• Use lowest dose, shortest duration
• Taper gradually
• Joint injections preferred
• Transition to steroid-sparing agents (MTX, biologics) ASAP
Never stop abruptly - adrenal suppression.
Physical and Occupational Therapy
Essential component of treatment!
Physical Therapy:
• Range of motion exercises - prevent stiffness
• Strengthening - support joints
• Stretching - maintain flexibility
• Hydrotherapy - pool exercises, gentle
• Pain management techniques
Occupational Therapy:
• Fine motor activities - hand function
• Daily living skills - dressing, eating
• Splints - rest joints, prevent deformity
• Joint protection techniques
• Adaptive equipment if needed
Goals:
• Maintain joint function
• Prevent contractures
• Maximize independence
• Return to normal activities
Frequency: Regular sessions - 2-3 times/week initially. Then home program.
Important: Exercise during remission too - prevent deconditioning.
Uveitis Treatment
Separate from joint treatment:
By Ophthalmologist:
• Topical steroids - eye drops
• Methotrexate - systemic
• Biologics - if resistant (Adalimumab approved)
• Mydriatic drops - prevent adhesions
Close monitoring: Can be sight-threatening. Aggressive treatment needed.
Often persists even when arthritis controlled! Lifelong screening needed.
SURGICAL TREATMENT
Surgery - When Needed?
Surgery is last resort in JIA. Modern medical treatment very effective - surgery much less common now than before biologics era. But still needed in some cases.
Synovectomy
Remove inflamed joint lining:
Indications:
• Persistent synovitis in single joint
• Despite medical treatment
• Risk of joint damage
• Pain affecting function
Procedure:
• Arthroscopic (keyhole) - preferred
• Remove inflamed synovium
• Knee most common
Outcomes:
• Pain relief
• Improved function
• May delay joint damage
• Not curative - can recur
Rare now - medical treatment usually controls.
Limb Length Correction
For leg length discrepancy:
Cause: In chronic arthritis - knee inflammation → overgrowth of that leg. OR undergrowth if very severe.
Significant discrepancy (>2-3 cm):
• Epiphysiodesis - stop growth of longer leg
• Limb lengthening - rare, complex
• Timing critical
Goal: Equal leg lengths at skeletal maturity.
Soft Tissue Releases
For contractures:
When joints get stuck:
• Flexion contractures - can't fully straighten
• Limited range of motion
• Affecting function
Procedures:
• Tendon lengthening
• Capsule release
• Joint manipulation
Post-op: Aggressive PT essential.
Joint Replacement (Arthroplasty)
For severe joint damage:
When:
• End-stage arthritis
• Severe pain
• Major functional limitation
• Failed medical treatment
• Skeletal maturity (usually wait till adult)
Joints:
• Hip - most common
• Knee
• Rarely - shoulder, ankle
Challenge in JIA:
• Young age - implants don't last forever
• May need revision surgeries later
• Try to delay as long as possible
Outcomes:
• Excellent pain relief
• Improved function
• Better quality of life
• Can return to many activities
Rare now - early aggressive medical treatment prevents this.
Eye Surgery
For uveitis complications:
Procedures:
• Cataract surgery - if cataract develops
• Glaucoma surgery - if high eye pressure
• Adhesion release - if iris stuck
By ophthalmologist: Specialized care needed.
TMJ (Jaw) Surgery
If jaw involved:
TMJ arthritis:
• Micrognathia (small jaw)
• Limited mouth opening
• Eating difficulties
Treatments:
• Distraction osteogenesis - lengthen jaw
• Joint replacement - severe cases
• Orthodontics
Complex: Multidisciplinary - orthodontist, maxillofacial surgeon.
Modern JIA Treatment - Success Story!
20-30 years ago: Many JIA children → wheelchair, severe disability, joint replacements.
TODAY with modern treatment:
• 50-70% achieve remission or near-remission
• 70-80% lead normal lives - school, sports, work
• Joint damage rare if treated early
• Surgery much less common
• Quality of life excellent
Key to success:
✅ Early diagnosis
✅ Aggressive treatment from start
✅ Regular monitoring
✅ Medication compliance
✅ Team approach - rheumatologist, ophthalmologist, PT, OT
✅ Family support
The message is HOPE! JIA is manageable. Children CAN thrive.
अक्सर पूछे जाने वाले सवाल (FAQ) Frequently Asked Questions (FAQ)
यह सबसे common और important सवाल है। Honest answer: JIA एक chronic autoimmune disease है - technically "cure" नहीं है। But यह पूरी story नहीं है! Remission - बहुत achievable! "Remission" means disease inactive - no symptoms, no active inflammation, normal life। Many children achieve remission और years तक remission में रहते हैं। Remission rates: • Oligoarticular JIA: 50-60% achieve remission। • Polyarticular JIA: 30-40% remission। • Systemic JIA: Variable - कुछ complete remission, कुछ chronic arthritis। Medications forever? Not necessarily! • If remission achieved और sustained (usually 1-2 years of stable disease off medications), medications can often be stopped। • Tapering approach: Gradually reduce medications। Monitor closely। • कुछ children medication-free years तक रहते हैं। • But some need low-dose maintenance। Reality check - scenarios: Best case (40-50% children): • Achieve remission on treatment। • Taper off medications gradually। • Remain medication-free। • Normal life। • May never flare again। • "Clinical cure" - even if technically disease can recur। Good case (30-40%): • Achieve remission on treatment। • Can reduce medications। • Need low-dose maintenance (like low-dose methotrexate once weekly)। • Normal life with minimal treatment। Challenging case (10-20%): • Difficult to control। • Need ongoing treatment। • May need biologics long-term। • But still functional life possible। Factors favoring remission: • Oligoarticular type। • Early diagnosis और treatment। • Good response to initial treatment। • ANA negative। • Compliance with treatment। • Regular monitoring। Important concepts: 1. "Cure" vs "Remission" - practical difference minimal! • If child is symptom-free, active, normal life - does label matter? • Focus on quality of life, not semantics। 2. Modern treatments improving outcomes: • Biologics era - much better remission rates। • Early aggressive treatment - prevents damage। • Many children NOW achieving "functional cure"। 3. Even if lifelong treatment needed: • Treatments safe। • Quality of life excellent। • Can do everything - school, sports, college, career, marriage। • Not wheelchair-bound ya disabled। Your child's journey - what to expect: First 6-12 months: • Finding right treatment। • Trial and adjustment। • Achieving disease control। Year 1-2: • Maintaining control। • Monitoring closely। • Adjusting as needed। Year 2-5: • If stable - discussing tapering। • Gradual medication reduction। • Close monitoring। Long-term: • Many medication-free। • Some low-dose maintenance। • Regular check-ups - ophthalmology especially। • Normal development। Key message: • Yes, JIA is chronic - but that doesn't mean "sick forever"! • Remission very achievable - majority achieve it। • Many children can stop medications eventually। • Even if long-term treatment needed - life is normal। • Focus on the POSITIVE: Your child CAN and WILL thrive! What YOU can do: ✅ Commit to treatment plan। ✅ Don't skip medications hoping disease will "go away"। ✅ Regular follow-ups। ✅ Stay hopeful - outcomes today are EXCELLENT! Remember: This is not the JIA of 20-30 years ago। Today's children with JIA have every reason to hope for normal, active, fulfilling lives!
This is the most common and important question. Honest answer: JIA is a chronic autoimmune disease - technically no "cure". But this isn't the full story! Remission - very achievable! "Remission" means disease inactive - no symptoms, no active inflammation, normal life. Many children achieve remission and stay in remission for years. Remission rates: • Oligoarticular JIA: 50-60% achieve remission. • Polyarticular JIA: 30-40% remission. • Systemic JIA: Variable - some complete remission, some chronic arthritis. Medications forever? Not necessarily! • If remission achieved and sustained (usually 1-2 years of stable disease off medications), medications can often be stopped. • Tapering approach: Gradually reduce medications. Monitor closely. • Some children remain medication-free for years. • But some need low-dose maintenance. Reality check - scenarios: Best case (40-50% children): • Achieve remission on treatment. • Taper off medications gradually. • Remain medication-free. • Normal life. • May never flare again. • "Clinical cure" - even if technically disease can recur. Good case (30-40%): • Achieve remission on treatment. • Can reduce medications. • Need low-dose maintenance (like low-dose methotrexate once weekly). • Normal life with minimal treatment. Challenging case (10-20%): • Difficult to control. • Need ongoing treatment. • May need biologics long-term. • But still functional life possible. Factors favoring remission: • Oligoarticular type. • Early diagnosis and treatment. • Good response to initial treatment. • ANA negative. • Compliance with treatment. • Regular monitoring. Important concepts: 1. "Cure" vs "Remission" - practical difference minimal! • If child is symptom-free, active, normal life - does label matter? • Focus on quality of life, not semantics. 2. Modern treatments improving outcomes: • Biologics era - much better remission rates. • Early aggressive treatment - prevents damage. • Many children NOW achieving "functional cure". 3. Even if lifelong treatment needed: • Treatments safe. • Quality of life excellent. • Can do everything - school, sports, college, career, marriage. • Not wheelchair-bound or disabled. Your child's journey - what to expect: First 6-12 months: • Finding right treatment. • Trial and adjustment. • Achieving disease control. Year 1-2: • Maintaining control. • Monitoring closely. • Adjusting as needed. Year 2-5: • If stable - discussing tapering. • Gradual medication reduction. • Close monitoring. Long-term: • Many medication-free. • Some low-dose maintenance. • Regular check-ups - ophthalmology especially. • Normal development. Key message: • Yes, JIA is chronic - but that doesn't mean "sick forever"! • Remission very achievable - majority achieve it. • Many children can stop medications eventually. • Even if long-term treatment needed - life is normal. • Focus on the POSITIVE: Your child CAN and WILL thrive! What YOU can do: ✅ Commit to treatment plan. ✅ Don't skip medications hoping disease will "go away". ✅ Regular follow-ups. ✅ Stay hopeful - outcomes today are EXCELLENT! Remember: This is not the JIA of 20-30 years ago. Today's children with JIA have every reason to hope for normal, active, fulfilling lives!
यह बहुत valid concern है! Let me address this completely। Yes, methotrexate (MTX) is used in cancer - लेकिन JIA में dose COMPLETELY different है! Dose comparison - crucial to understand: Cancer treatment: • High doses - 100-1000+ mg। • Daily या multiple times per week। • Short duration - few months। • Severe side effects expected। JIA treatment: • Low doses - 10-25 mg। • ONCE per week। • Long duration - years। • Side effects minimal at these doses। This is like comparing: • Aspirin for heart attack prevention (low dose, daily, safe)। • vs Aspirin overdose (high dose, toxic)। • Same drug, different dose = completely different safety profile! Safety data in JIA - EXTENSIVE: • 40+ years of use in children with JIA। • Thousands of children treated worldwide। • Well-established safety profile। • Benefits far outweigh risks at JIA doses। Common side effects (most children tolerate well): 1. Nausea (30-40% children): • Usually mild। • Day after dose। • Management: - Take at bedtime - sleep through nausea। - Anti-nausea medication before dose। - Injectable form better tolerated than oral। - Ginger candies। - Usually improves with time। 2. Mouth sores (10-20%): • Mild। • Prevention: Folic acid supplementation (ALWAYS given with MTX) - reduces mouth sores by 70%! 3. Hair thinning (rare, <5%): • NOT hair loss like chemotherapy! • Minimal thinning। • Reversible। 4. Fatigue: • Day after dose। • Mild। • Resolves। Less common side effects (monitored with blood tests): 5. Liver enzyme elevation (10-15%): • Usually asymptomatic। • Detected on blood tests। • Monitoring: Blood tests every 4-8 weeks। • If elevated - may reduce dose या temporarily stop। • Usually reversible। 6. Blood count changes (rare): • Mild decrease in WBC या platelets। • Monitored। • Rarely requires stopping drug। What about long-term effects? Cancer risk: • NO increased cancer risk at JIA doses। • This is cancer chemotherapy concern, NOT JIA treatment concern। Fertility: • NO effect on future fertility at JIA doses। • Can have normal children later। • May need to stop before pregnancy planning (females) - discuss with doctor। Growth: • Does NOT affect growth। • In fact, controlling JIA with MTX allows NORMAL growth (uncontrolled JIA impairs growth)। Liver damage: • Long-term liver damage VERY rare। • Much lower risk than uncontrolled JIA। • Monitoring catches any issues early। Comparing risks - perspective: Risk of MTX side effects requiring stopping drug: • 5-10%। Risk of permanent disability if JIA untreated: • 50-70%! The REAL risk is NOT treating! Monitoring protocol - ensures safety: • Blood tests every 4-8 weeks - liver, kidneys, blood counts। • Any abnormalities detected early। • Dose adjusted or stopped if needed। • Close follow-up। Safety measures - maximize safety: ✅ Folic acid: ALWAYS take - 5-7 days/week (not on MTX day)। Reduces side effects। ✅ Avoid alcohol: No alcohol (not issue in children, but important for teens/adults)। ✅ Regular blood tests: Don't skip! ✅ Report symptoms: Severe nausea, vomiting, rash, fever, easy bruising। ✅ Avoid NSAIDs same day: Take NSAIDs different day if possible। ✅ No live vaccines: While on MTX। When methotrexate is AMAZING: • 60-70% children respond well - significant improvement। • Prevents joint damage - saves joints! • Allows normal life - school, play, sports। • Avoids steroids - which have WORSE side effects। • Delays/avoids biologics - more expensive, injections। Real-world parent experiences: Common story: "We were terrified of MTX। Delayed starting। Child suffered। Finally started - minimal side effects, dramatic improvement। Wish we'd started earlier!" Alternative perspective - what if you DON'T use MTX: • Uncontrolled inflammation। • Progressive joint damage। • Disability। • Need for more aggressive treatment later। • Irreversible damage। My recommendation as doctor: Methotrexate is: ✅ Gold standard for JIA। ✅ Safe at JIA doses। ✅ Well-tolerated by most children। ✅ Prevents disability। ✅ Decades of safety data। Your fear is understandable - it's a strong drug। But at JIA doses, it's a safe, effective, life-changing medication for your child। Trust the data, not the fear! Actionable advice: • Start MTX as prescribed। • Give folic acid daily। • Do blood tests regularly। • Report side effects। • Give it 12 weeks - takes time to work। • Vast majority tolerate well। Remember: You're not giving your child "chemotherapy" - you're giving a carefully dosed, well-monitored, proven medication that will protect their joints and give them a normal childhood!
This is very valid concern! Let me address this completely. Yes, methotrexate (MTX) is used in cancer - but in JIA the dose is COMPLETELY different! Dose comparison - crucial to understand: Cancer treatment: • High doses - 100-1000+ mg. • Daily or multiple times per week. • Short duration - few months. • Severe side effects expected. JIA treatment: • Low doses - 10-25 mg. • ONCE per week. • Long duration - years. • Side effects minimal at these doses. This is like comparing: • Aspirin for heart attack prevention (low dose, daily, safe). • vs Aspirin overdose (high dose, toxic). • Same drug, different dose = completely different safety profile! Safety data in JIA - EXTENSIVE: • 40+ years of use in children with JIA. • Thousands of children treated worldwide. • Well-established safety profile. • Benefits far outweigh risks at JIA doses. Common side effects (most children tolerate well): 1. Nausea (30-40% children): • Usually mild. • Day after dose. • Management: - Take at bedtime - sleep through nausea. - Anti-nausea medication before dose. - Injectable form better tolerated than oral. - Ginger candies. - Usually improves with time. 2. Mouth sores (10-20%): • Mild. • Prevention: Folic acid supplementation (ALWAYS given with MTX) - reduces mouth sores by 70%! 3. Hair thinning (rare, <5%): • NOT hair loss like chemotherapy! • Minimal thinning. • Reversible. 4. Fatigue: • Day after dose. • Mild. • Resolves. Less common side effects (monitored with blood tests): 5. Liver enzyme elevation (10-15%): • Usually asymptomatic. • Detected on blood tests. • Monitoring: Blood tests every 4-8 weeks. • If elevated - may reduce dose or temporarily stop. • Usually reversible. 6. Blood count changes (rare): • Mild decrease in WBC or platelets. • Monitored. • Rarely requires stopping drug. What about long-term effects? Cancer risk: • NO increased cancer risk at JIA doses. • This is cancer chemotherapy concern, NOT JIA treatment concern. Fertility: • NO effect on future fertility at JIA doses. • Can have normal children later. • May need to stop before pregnancy planning (females) - discuss with doctor. Growth: • Does NOT affect growth. • In fact, controlling JIA with MTX allows NORMAL growth (uncontrolled JIA impairs growth). Liver damage: • Long-term liver damage VERY rare. • Much lower risk than uncontrolled JIA. • Monitoring catches any issues early. Comparing risks - perspective: Risk of MTX side effects requiring stopping drug: • 5-10%. Risk of permanent disability if JIA untreated: • 50-70%! The REAL risk is NOT treating! Monitoring protocol - ensures safety: • Blood tests every 4-8 weeks - liver, kidneys, blood counts. • Any abnormalities detected early. • Dose adjusted or stopped if needed. • Close follow-up. Safety measures - maximize safety: ✅ Folic acid: ALWAYS take - 5-7 days/week (not on MTX day). Reduces side effects. ✅ Avoid alcohol: No alcohol (not issue in children, but important for teens/adults). ✅ Regular blood tests: Don't skip! ✅ Report symptoms: Severe nausea, vomiting, rash, fever, easy bruising. ✅ Avoid NSAIDs same day: Take NSAIDs different day if possible. ✅ No live vaccines: While on MTX. When methotrexate is AMAZING: • 60-70% children respond well - significant improvement. • Prevents joint damage - saves joints! • Allows normal life - school, play, sports. • Avoids steroids - which have WORSE side effects. • Delays/avoids biologics - more expensive, injections. Real-world parent experiences: Common story: "We were terrified of MTX. Delayed starting. Child suffered. Finally started - minimal side effects, dramatic improvement. Wish we'd started earlier!" Alternative perspective - what if you DON'T use MTX: • Uncontrolled inflammation. • Progressive joint damage. • Disability. • Need for more aggressive treatment later. • Irreversible damage. My recommendation as doctor: Methotrexate is: ✅ Gold standard for JIA. ✅ Safe at JIA doses. ✅ Well-tolerated by most children. ✅ Prevents disability. ✅ Decades of safety data. Your fear is understandable - it's a strong drug. But at JIA doses, it's a safe, effective, life-changing medication for your child. Trust the data, not the fear! Actionable advice: • Start MTX as prescribed. • Give folic acid daily. • Do blood tests regularly. • Report side effects. • Give it 12 weeks - takes time to work. • Vast majority tolerate well. Remember: You're not giving your child "chemotherapy" - you're giving a carefully dosed, well-monitored, proven medication that will protect their joints and give them a normal childhood!
YES! Sports ENCOURAGED! Swimming (BEST - low-impact), cycling, yoga, dancing, team sports usually fine! School PE - participate with modifications during flares, full participation in remission. Exercise doesn't damage controlled joints - actually protective! Tips: warm-up, good shoes, hydrate, don't skip meds. Modify if pain increases. JIA NOT reason to avoid sports! Physical activity ESSENTIAL.
YES! Sports ENCOURAGED! Swimming (BEST), cycling, yoga, dancing, team sports usually fine! School PE - participate with modifications during flares. Exercise doesn't damage controlled joints - protective! Tips: warm-up, good shoes, hydrate. Modify if pain increases. Physical activity ESSENTIAL for JIA!
CRITICAL! Uveitis (eye inflammation) often SILENT - no symptoms initially! Only detected by slit-lamp exam. 10-20% JIA children develop it. Can cause blindness if untreated. Screening protocol: High risk (oligoarticular, ANA+) - every 3 months! Lifelong - even in remission. Must be ophthalmologist with slit-lamp, not regular eye doctor. Early detection saves vision!
CRITICAL! Uveitis often SILENT - no symptoms! Only detected by slit-lamp. 10-20% get it. Can cause blindness. High risk: screen every 3 months! Lifelong. Must be ophthalmologist. Early detection saves vision!
Good news: 60-70% respond to methotrexate alone (₹2000-4000/month)! Try MTX first. If biologics needed: (1) Insurance coverage - most cover with prior authorization, (2) Patient assistance programs - pharma companies offer (Pfizer, AbbVie), income-based, can be FREE, (3) Biosimilars - 30-50% cheaper, (4) Government schemes, (5) Crowdfunding. Don't skip treatment due to cost - disability costs more! Early treatment saves long-term. Explore ALL options - help available!
60-70% respond to methotrexate alone (affordable)! If biologics needed: Insurance, patient assistance programs (can be free!), biosimilars (30-50% cheaper), government schemes, crowdfunding. Don't skip treatment - explore all options!
Get doctor's letter! Meet with teachers. Request accommodations: Extra time for exams, laptop for notes, modified PE, flexible arrival (morning stiffness), locker access, reduced homework. Educate teachers - JIA is real, invisible illness, fluctuating. If resistant: Meet principal, more documentation, know rights - accommodations are RIGHTS not privileges. Most teachers cooperative once they understand!
Doctor's letter! Meet teachers. Accommodations: Extra time, laptop, modified PE, flexible arrival, locker. Educate teachers. If resistant - principal, documentation, know rights. Accommodations are RIGHTS!
Partially genetic but NOT straightforward. Siblings risk: 2-5% (vs 0.1% general population). But 95-98% chance siblings WON'T get JIA! Don't avoid pregnancy - risk small. If YOU have JIA and planning pregnancy: stop methotrexate 3-6 months before, plan with rheumatologist. Most JIA women have normal pregnancies. Genetic testing NOT useful. Prevention NOT possible. Monitor siblings for symptoms but live your life!
Partially genetic. Siblings risk 2-5%. 95-98% won't get JIA! Don't avoid pregnancy. If you have JIA: plan medications before pregnancy. Most have normal pregnancies. Monitor siblings but live your life!
Emotional health AS important as physical! Common challenges: feeling different, social isolation, bullying. Actions: (1) Professional counseling - child psychologist, CBT effective, (2) Peer support groups - "not alone", (3) Validate feelings, (4) Address bullying immediately with school, (5) Build resilience - focus on strengths. URGENT if: Suicidal thoughts, self-harm - get emergency help! Parent self-care critical - can't pour from empty cup. Mental health support = better outcomes!
Mental health AS important! Actions: Professional counseling, peer support, validate feelings, address bullying with school, build resilience. URGENT if suicidal thoughts! Parent self-care critical. Mental + physical support = best outcomes!
Yoga - BENEFICIAL! ✅ As ADDITION to medical treatment. Diet - anti-inflammatory may help slightly, NOT cure. Ayurveda - CAUTION! No scientific evidence, herb-drug interactions, delay of proven treatment. Homeopathy - NO EVIDENCE! Wastes time/money. What IS proven: NSAIDs, methotrexate, biologics. Integrative approach BEST: Medical treatment as foundation PLUS complementary (yoga, healthy diet, massage). Beware "miracle cures"! Don't delay proven treatment - permanent damage happens!
Yoga - beneficial as ADDITION! Diet may help slightly. Ayurveda/homeopathy - no evidence. Proven: NSAIDs, methotrexate, biologics. Best approach: Medical foundation + complementary. Don't delay proven treatment!
YES! Completely normal life possible! With modern treatment: 50-70% achieve remission, 70-80% functional independence, NORMAL lifespan! EDUCATION: Can do college, professional degrees - ANYTHING! CAREER: Almost all suitable - IT, medicine, law, teaching. MARRIAGE: Absolutely! CHILDREN: JIA doesn't affect fertility. Plan medications before pregnancy. Most have normal pregnancies. Key: Early diagnosis, early treatment, compliance. Future is BRIGHT! "You have JIA. JIA doesn't have you!"
YES! Normal life possible! 50-70% remission. EDUCATION: anything! CAREER: almost all. MARRIAGE: yes! CHILDREN: plan medications, most normal pregnancies. Future BRIGHT with modern treatment!
Morning stiffness hallmark of JIA! Immediate relief: Warm bath/shower first thing, gentle ROM exercises before getting up, heat packs. Medications: Give NSAIDs at bedtime (works overnight), methotrexate - takes weeks but improves stiffness. Physical therapy: Night splints, positioning. School: Flexible arrival time. Long-term: Better disease control = less stiffness. Biologics very effective for severe stiffness. Sign of active disease - tell rheumatologist, may need treatment adjustment!
Morning stiffness is hallmark! Immediate: warm bath, gentle exercises, heat. Medications: NSAIDs at bedtime. PT: night splints. School: flexible arrival. Long-term: better control = less stiffness. Tell rheumatologist!
Most vaccines SAFE and IMPORTANT! CAN give: Inactivated vaccines (flu, COVID, hepatitis, polio, diphtheria-tetanus). CANNOT give LIVE vaccines: MMR, varicella, rotavirus - while on methotrexate या biologics. Give live vaccines BEFORE starting immunosuppression if possible. COVID vaccine: YES, recommended! Higher infection risk on meds. May have slightly reduced response but still protective. Timing: Hold biologics 1-2 weeks around vaccination for better response (discuss with doctor). Family members should be fully vaccinated too - protect child!
Most vaccines SAFE! CAN: inactivated (flu, COVID, hepatitis). CANNOT: live vaccines (MMR, varicella) on methotrexate/biologics. COVID vaccine: YES, recommended! Timing: may hold biologics around vaccination. Family should vaccinate too!
अपॉइंटमेंट बुक करें
Book Your Appointment
Juvenile Rheumatoid Arthritis के expert diagnosis और comprehensive treatment के लिए
Dr. Gaurav Jain से आज ही संपर्क करें।
For expert diagnosis and comprehensive treatment of Juvenile Rheumatoid Arthritis
Contact Dr. Gaurav Jain today.